
 النبات
النبات
 الحيوان
الحيوان
 الأحياء المجهرية
الأحياء المجهرية
 علم الأمراض
علم الأمراض
 التقانة الإحيائية
التقانة الإحيائية
 التقنية الحيوية المكروبية
التقنية الحيوية المكروبية
 التقنية الحياتية النانوية
التقنية الحياتية النانوية
 علم الأجنة
علم الأجنة
 الأحياء الجزيئي
الأحياء الجزيئي
 علم وظائف الأعضاء
علم وظائف الأعضاء
 الغدد
الغدد
 المضادات الحيوية
المضادات الحيوية|
Read More
Date: 27-7-2021
Date: 1-8-2021
Date: 15-7-2021
|
Temporal Region
The temporal region is located laterally on the skull and includes both the temporal and infratemporal fossae (Fig. 1). This region contains muscles of mastication, branches of the mandibular division of the trigeminal nerve (CN V3), and terminal branches of the external carotid artery.

Figure 1: Temporal region.
A. Temporal fossa
The temporal fossa is bound by the superior and inferior temporal lines posteriorly and superiorly, frontal and zygomatic bones anteriorly, infratemporal crest inferiorly, and the zygomatic arch laterally. The temporalis muscle fills the majority of this bound space, projecting inferiorly into the infratemporal fossa. The bony intersection known as the pterion is contained within the temporal fossa.
B. lnfratemporal fossa
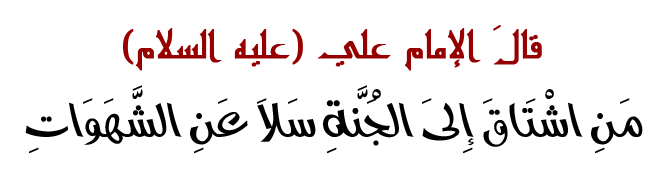
The infratemporal fossa lies inferior to the zygomatic arch and is bound anteriorly by the posterior maxilla, posteriorly by the condylar process of the mandible, medially by the lateral pterygoid plate, laterally by the ram us of the mandible, and superiorly by the infratemporal crest (Figs. 2 and 3). Inferiorly, the space is closed by the medial pterygoid muscle. The contents of the infratemporal fossa include the maxillary artery and branches, the mandibular division of the trigeminal nerve (CN V3) and branches, the pterygoid venous plexus, medial and lateral pterygoid muscles and the inferior portion of the temporalis muscle, the otic ganglion, and the chorda tympani nerve (branch of CN VII).
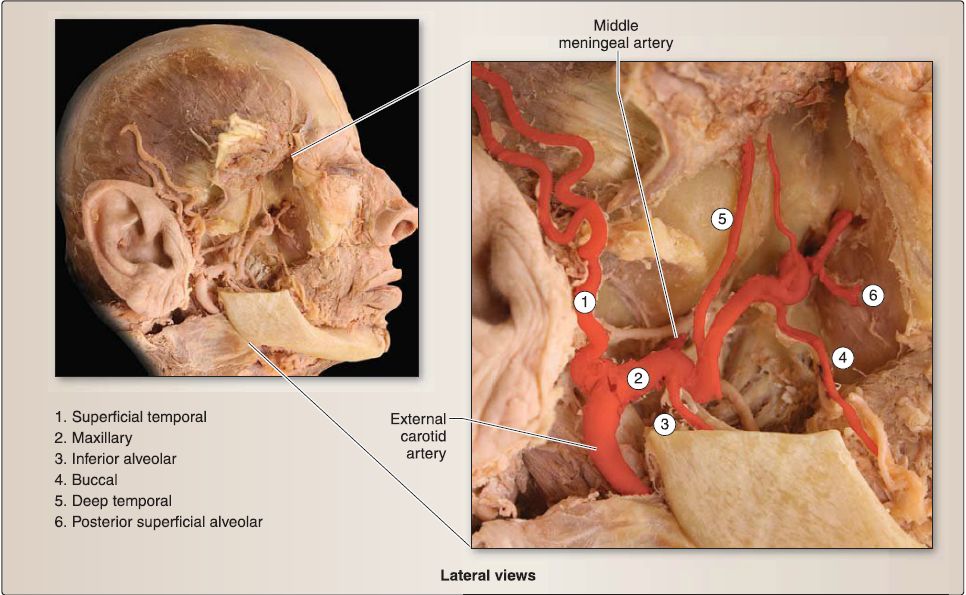 Figure 2: lnfratemporal fossa: maxillary artery and branches (lateral pterygoid and masseter muscles, mandibular condyle, coronoid process, and ramus removed; temporalis reflected superiorly).
Figure 2: lnfratemporal fossa: maxillary artery and branches (lateral pterygoid and masseter muscles, mandibular condyle, coronoid process, and ramus removed; temporalis reflected superiorly).
 Figure 3: lnfratemporal fossa: maxillary division of trigeminal nerve ,Y3). (Lateral pterygoid and masseter muscles, mandibular condyle, coronoid process, and ramus removed; temporalis reflected superiorly.)
Figure 3: lnfratemporal fossa: maxillary division of trigeminal nerve ,Y3). (Lateral pterygoid and masseter muscles, mandibular condyle, coronoid process, and ramus removed; temporalis reflected superiorly.)
1. Maxillary artery: The maxillary artery, a terminal branch of the external carotid artery, travels deep to the neck of the mandible to (TMJ), external ear, meninges, lower jaw and teeth, and muscles of mastication. The terminal part of the maxillary artery travels into the pterygopalatine fossa to serves structures of the palate, nasal cavity, and upper jaw and teeth. Of clinical significance is the middle meningeal artery branch that travels into the middle cranial fossa through the foramen spinosum. This vessel travels deep to the pterion and is a great risk for damage and subsequent epidural hematoma .
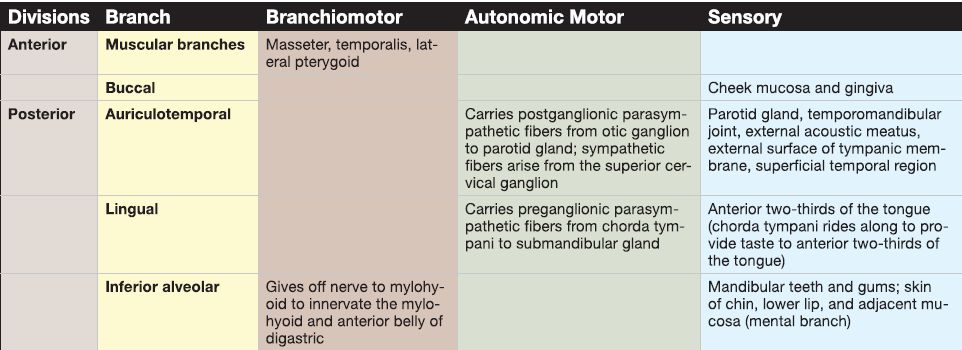
2. Mandibular division of the trigeminal nerve: CN V3 enters the infratemporal fossa through the foramen ovale, where it divides into anterior (mainly motor) and posterior (mainly sensory) divisions. Prior to dividing, CN V3 gives off a small sensory branch (spinous nerve) to the dura and lining of the mastoid cells and a small branchiomotor branch to the medial pterygoid muscle. The motor branches of CN V3 provide branchiomotor innervation to the muscles of mastication, mylohyoid, and anterior belly of the digastric muscle. The main sensory nerves of CN V3 include:
a. Lingual nerve: The lingual nerve continues into the oral cavity, where it is anatomically associated with the submandibular ganglion. This relationship is further discussed in the "Oral cavity" section. enter the infratemporal fossa. Within the fossa, it gives off a number of branches that serve structures of the temporomandibular joint b. Inferior alveolar nerve: After giving off the nerve to mylohyoid, the inferior alveolar nerve enters the mandibular foramen to travel through the lower jaw. It exits through the mental foramen to the face and is renamed the mental nerve.
c. Buccal nerve: The buccal nerve travels anteriorly in the infratemporal fossa to enter the oral cavity and provide sensory innervation to the mucosa of the cheek. Do not confuse this nerve with the buccal branch of the facial nerve.
3. Otic ganglion: The otic ganglion lies high in the fossa, medially to and anatomically associated with CN V3• Details are listed in Table 1.
Table 1: Mandibular Division of Trigeminal Nerve (CN V3) Branches Divisions Branch Branchiomotor Autonomic Motor Sensory
C. Muscles of mastication
The muscles of mastication include the temporalis, masseter, and medial and lateral pterygoid muscles (Fig. 4). Collectively, they function to assist with chewing food. They act on the TMJ, to impart movement to the mandible. All four muscles receive branchiomotor innervation from CN V3•
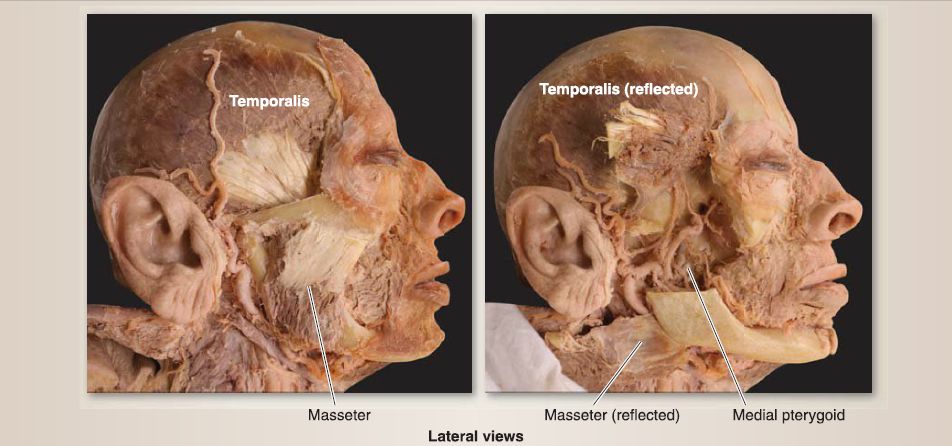 Figure 4: Muscles of mastication. (Zygomatic arch, mandibular condyle, coronoid process, ramus, and lateral pterygoid muscle removed in right image.)
Figure 4: Muscles of mastication. (Zygomatic arch, mandibular condyle, coronoid process, ramus, and lateral pterygoid muscle removed in right image.)
1. Temporalis: This muscle originates from temporal fossa and inserts onto the coronoid process of the mandible. It functions to elevate and retract (posterior fibers) the mandible.
2. Masseter: This muscle originates from the zygomatic arch and inserts onto the lateral surface of the mandibular ramus. It functions to elevate, protrude, and retract (deep fibers) the mandible.
3. Medial pterygoid: This muscle originates from the medial surface of the lateral pterygoid plate, posterolateral palatine bone, and maxillary tubercle and inserts onto the medial surface of the mandibular ramus. It functions bilaterally to elevate and protrude the mandible and unilaterally and alternating to produce a side-to-side grinding motion.
4. Lateral pterygoid: This muscle originates from the infratemporal crest and lateral surface of the lateral pterygoid plate and inserts onto the mandibular neck and TMJ capsule. Like the medial pterygoid, it functions bilaterally to protrude the mandible and unilaterally and alternating to produce a side-to-side grinding motion.
5. Temporomandibular joint: The TMJ occurs between the head of the mandible and the mandibular fossa and articular tubercle of the temporal bone (Fig. 5). This synovial joint is enclosed in a loose joint capsule, which contains an articular disc and supporting internal ligaments. The TMJ is a triplanar joint that allows for elevation, depression, protrusion, retraction, and side-to-side movements of the mandible.
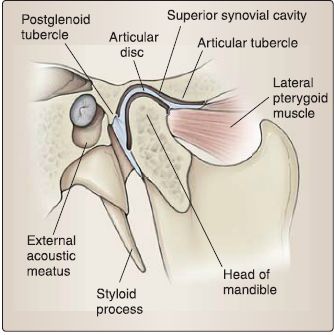
Figure 5: Temporomandibular joint (fMJ).



|
|
|
|
التوتر والسرطان.. علماء يحذرون من "صلة خطيرة"
|
|
|
|
|
|
|
مرآة السيارة: مدى دقة عكسها للصورة الصحيحة
|
|
|
|
|
|
|
نحو شراكة وطنية متكاملة.. الأمين العام للعتبة الحسينية يبحث مع وكيل وزارة الخارجية آفاق التعاون المؤسسي
|
|
|