
 النبات
النبات
 الحيوان
الحيوان
 الأحياء المجهرية
الأحياء المجهرية
 علم الأمراض
علم الأمراض
 التقانة الإحيائية
التقانة الإحيائية
 التقنية الحيوية المكروبية
التقنية الحيوية المكروبية
 التقنية الحياتية النانوية
التقنية الحياتية النانوية
 علم الأجنة
علم الأجنة
 الأحياء الجزيئي
الأحياء الجزيئي
 علم وظائف الأعضاء
علم وظائف الأعضاء
 الغدد
الغدد
 المضادات الحيوية
المضادات الحيوية|
Read More
Date: 9-7-2021
Date: 30-7-2021
Date: 5-11-2015
|
Fascia, Vasculature, Lymphatics, and Innervation
Many structures in the lower limb can be described as either superficial or deep, including fascial layers, venous vessels, and lymphatic vessels and nodes. The following section describes the organization of these structures in addition to the arterial and nervous supply of the lower limb.
A. Superficial fascia
Deep to the skin of the lower limb lies a superficial fascia that contains varying amounts of loose connective and adipose tissues. Superficial veins, lymphatic vessels, and cutaneous nerves travel in this fascia, which is continuous with the superficial fascia of the abdomen.
B. Deep fascia
Deep to the superficial fascia is a thick, strong fascia that aids in venous blood return to the heart from the lower limbs by improving the efficiency of muscle contraction. The deep fascia of the thigh (fascia lata) and leg (crural fascia) are continuous with each other and collectively invest the lower limb muscle compartments (Fig. 1).
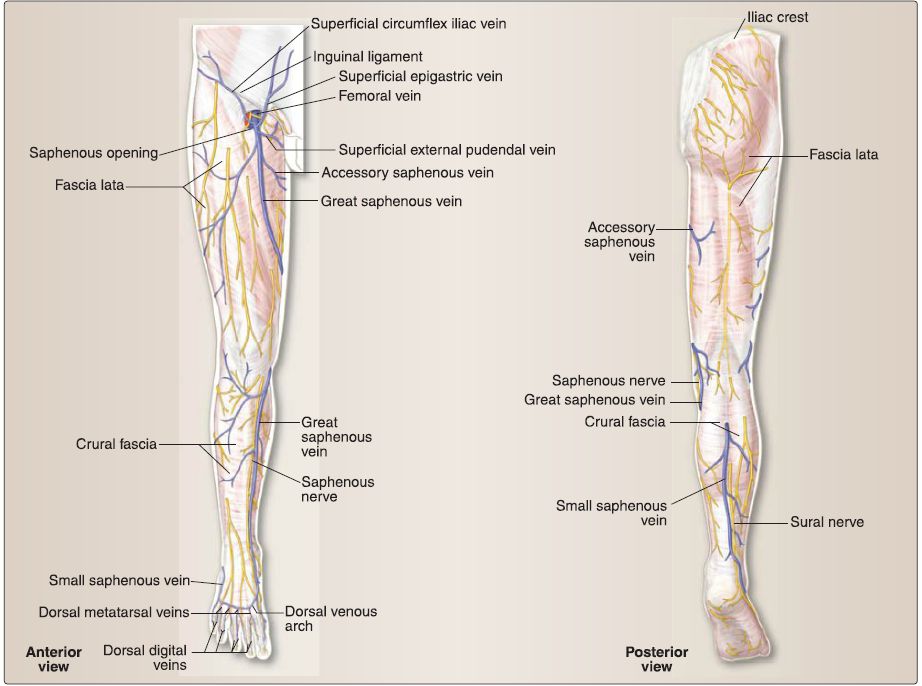
Figure 1: Deep fascia and superficial veins of the lower limb.
1. Saphenous opening: Proximally, the fascia lata is continuous with the deep fascia of the gluteal region, inguinal ligament, and membranous fascia of the abdomen (Scarpa fascia). There is an opening in the fascia lata over the femoral triangle region called the saphenous opening, which allows for the great saphenous vein to drain into the femoral vein.
2. lliotibial tract: Laterally, the fascia lata thickens into a band of connective tissue called the iliotibial tract (or band), which runs from the ilium to the tibia. The gluteus maximus and tensor fasciae latae muscles use the iliotibial tract as a shared distal tendon.
3. Fascial intermuscular septa: These project internally to attach to bone and create the rigid compartments of the thigh (anterior, medial, posterior) and leg (anterior, lateral, posterior).
C. Venous drainage
Venous drainage of the lower limb occurs through a superficial and deep venous network (Fig. 2). Superficial and perforating veins have valves to ensure-under normal conditions-unidirectional blood return.

Figure 2 :Venous drainage of the lower limb. Only deep and superficial veins of the leg are shown; deep veins of the thigh (not shown) correspond in course and name to lower limb arteries. Arrows indicate direction of blood flow. MM = medial malleolus, P = patella, PV = perforating vein.
1. Superficial veins: The great saphenous vein and small saphenous vein travel superiorly from the dorsum of the foot to drain into more proximal, deep veins-femoral and popliteal, respectively. Multiple, small tributary veins drain into these two main superficial veins.
The great saphenous vein travels anterior to the medial malleolus, posterior to the medial femoral condyle, and then courses up the medial thigh before emptying into the femoral vein by way of the saphenous opening in the fascia lata. The small saphenous vein travels posterior to the lateral malleolus and courses up the posterior leg before piercing the crural fascia to empty into the popliteal vein in the popliteal fossa.
2. Multiple perforating veins: These pierce the deep fascia of the lower limb along the course of the superficial veins to connect superficial to deep veins.
3. Deep veins: In the lower limb, these travel with all major lower limb arteries and branches and typically carry the same name. In the leg, a pair of veins often accompanies a single artery.
D. Lymphatics
Lymphatics of the lower limb are closely associated with the venous system (Fig. 3).
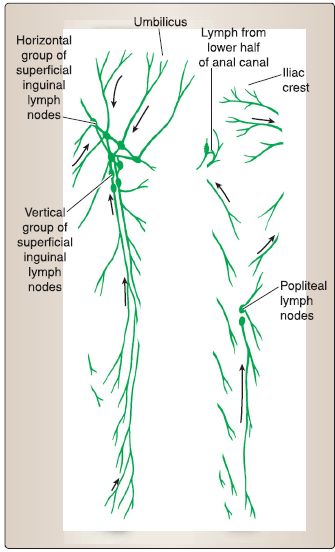
Figure 3: Lymphatics of the lower limb. Arrows indicate direction of lymph flow.
1. Superficial: Superficial lymphatic vessels travel with the saphenous vessels and drain into associated lymph nodes. Lymphatics that travel with the great saphenous vein drain into superficial inguinallymph nodes (vertical group) first before draining into external iliac nodes. Those that travel with the small saphenous vein drain directly into the popliteal nodes.
2. Deep: Lymphatic vessels also travel with deep veins in the leg, which first drain into popliteal nodes, then into deep inguinal nodes, and external and common iliac nodes, and finally the lumbar lymphatic trunks.
E. Arterial supply
The lower limb receives arterial blood supply primarily from the femoral artery and its branches (Fig. 4). Additionally, the gluteal region is supplied by superior and inferior gluteal arteries, and the medial thigh by the obturator artery, which are all branches from the internal iliac artery system. The obturator artery also gives off a small acetabular branch to the head of the femur.
 Figure 4: Arterial supply of the lower limb.
Figure 4: Arterial supply of the lower limb.
1. Femoral artery: After passing deep to the inguinal ligament, the external iliac artery is renamed as the femoral artery, which lies between the femoral nerve and vein in the femoral triangle. Within the femoral triangle, the femoral artery gives off three superficial branches (superficial epigastric, superficial circumflex iliac, and superficial external pudendal).
2. Profunda femoris artery: The main branch of the femoral artery is the profunda femoris artery, which travels between the pectineus and adductor longus muscles to descend adjacent to the femur.
Along its course, the profunda femoris artery gives off lateral and medial femoral circumflex arteries as well as three to four perforating arteries, which travel posteriorly to supply structures in the posterior thigh compartment.
a. Lateral femoral circumflex artery: This artery has three main branches-ascending, transverse, and descending. The transverse branch anastomoses with the medial femoral circumflex artery, to supply the head and neck of the femur (intercapsular), while the descending branch supplies much of the lateral thigh and contributes to collateral blood supply to the knee.
b. Medial femoral circumflex artery: This is the main artery to the hip joint.
3. Popliteal artery: After giving off superficial and deep branches, the femoral artery supplies adjacent structures as it travels inferiorly in the adductor canal of the anterior thigh compartment. Once the femoral artery reaches and passes through the adductor hiatus (musculotendinous opening in the adductor magnus muscle), it is renamed the popliteal artery.
The popliteal artery is found deep in the popliteal fossa where it gives off geniculate branches to supply the knee joint. It crosses the knee joint and divides into anterior and posterior tibial arteries, which travel to anterior and posterior leg compartments, respectively.
a. Posterior tibial artery: This artery gives off a fibular artery branch, which supplies blood to both the posterior and lateral leg compartments. The posterior tibial artery courses distally and travels posterior to the medial malleolus where it divides into medial plantar (MP) and lateral plantar (LP) arteries. Plantar arteries supply the plantar surface of the foot. The LP artery continues as the deep plantar arch artery, which eventually anastomoses with the deep plantar artery.
b. Anterior tibial artery: This artery continues distally in the anterior leg compartment and crosses the ankle joint, at which point it is renamed dorsalis pedis artery. Main branches of the dorsalis pedis artery serve the dorsum of the foot and include the lateral tarsal artery, arcuate artery, first posterior metatarsal artery, and the deep plantar artery.
c. Digital arteries: These arise from both the arcuate and deep plantar arch arteries to supply the toes.
F. Innervation
The lumbar and sacral nerve plexuses-collectively referred to as the lumbosacral plexus-provide general somatic afferent (sensory) and efferent (motor) innervation to all lower limb structures (Fig. 5).
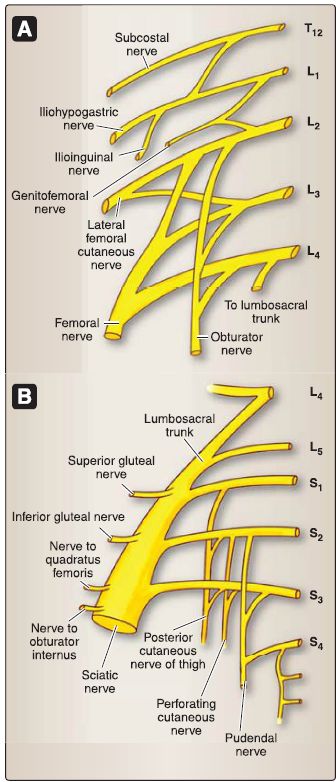
Figure 5: A, Lumbar plexus. B, Sacral plexus.
1. Terminal nerves: The lumbar and sacral plexuses contain anterior rami from L1-L4 and Ls, S1-S4, respectively. Rami divide into anterior and posterior divisions (pre- and postaxial, respectively) before forming terminal nerves. Although most terminal nerves are made up of anterior or posterior divisions, the sciatic nerve and posterior femoral cutaneous nerve have both anterior and posterior division components.
The five main terminal nerves (and their branches) of the lumbosacral plexus are:
• Femoral nerve, posterior divisions (L2-L4)
• Obturator nerve, anterior divisions (L2-L4)
• Superior gluteal nerve, posterior divisions (LcLs, S1)
• Inferior gluteal nerve, posterior divisions (Ls, S1-S2)
• Sciatic nerve, anterior and posterior divisions (LcLs, S1-S3)
• Common fibular nerve, posterior divisions (LcLs, S1-S2)
• Superficial fibular nerve
• Deep fibular nerve
• Tibial nerve, anterior divisions (LcLs, S1-S3)
• LP nerve
• MP nerve
Cutaneous innervation (Fig. 6) of the lower limb is primarily relayed by branches of the main terminal nerves, as well as lateral femoral cutaneous (L2-L3), genitofemoral (L1-L2), ilioinguinal (L1), posterior femoral cutaneous (S1-S3), and
clunial nerves (L1-L3; S1-S3).
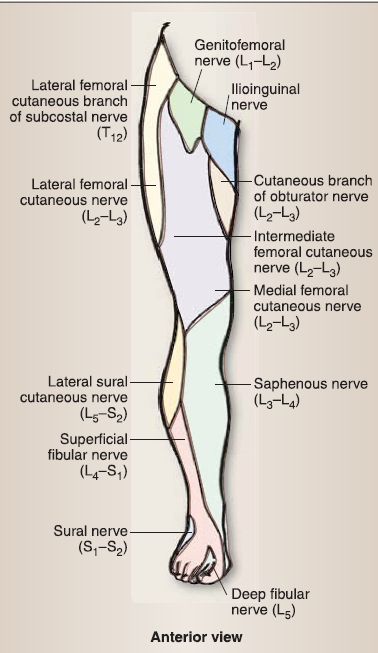
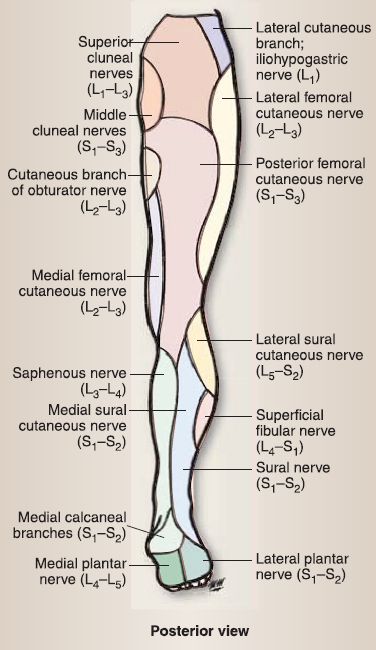
Figure 6: Cutaneous innervation maps for the lower limb.
2. Nerves to lateral rotators: The lumbosacral plexus also gives rise to smaller nerves that innervate the hip joint and muscles of the gluteal region. These include nerve to quadratus femoris and inferior gemellus (L4-L5, S1), nerve to piriformis (S1-S2), and nerve to obturator internus and superior gemellus (L5, S1-S2).
3. Pelvic splanchnic nerves: In addition, the sacral plexus gives rise to pelvic splanchnic nerves (S2-S4), which provide general visceral afferent (GVA) and general visceral efferent (GVE) parasympathetic innervation to structures in the pelvis and perineum (. Postganglionic sympathetic fibers travel with terminal nerves to provide GVA and GVE innervation to lower limb vasculature and glands.



|
|
|
|
التوتر والسرطان.. علماء يحذرون من "صلة خطيرة"
|
|
|
|
|
|
|
مرآة السيارة: مدى دقة عكسها للصورة الصحيحة
|
|
|
|
|
|
|
نحو شراكة وطنية متكاملة.. الأمين العام للعتبة الحسينية يبحث مع وكيل وزارة الخارجية آفاق التعاون المؤسسي
|
|
|