


 النبات
النبات
 الحيوان
الحيوان
 الأحياء المجهرية
الأحياء المجهرية
 علم الأمراض
علم الأمراض
 التقانة الإحيائية
التقانة الإحيائية
 التقنية الحيوية المكروبية
التقنية الحيوية المكروبية
 التقنية الحياتية النانوية
التقنية الحياتية النانوية
 علم الأجنة
علم الأجنة
 الأحياء الجزيئي
الأحياء الجزيئي
 علم وظائف الأعضاء
علم وظائف الأعضاء
 الغدد
الغدد
 المضادات الحيوية
المضادات الحيوية|
Read More
Date: 2-11-2021
Date: 30-11-2021
Date: 27-9-2021
|
Porphyrias
Porphyrias are rare, inherited (or sometimes acquired) defects in heme synthesis, resulting in the accumulation and increased excretion of porphyrins or porphyrin precursors . [Note: Inherited porphyrias are autosominal-dominant (AD) or autosomal-recessive (AR) disorders.] Each porphyria results in the accumulation of a unique pattern of intermediates caused by the deficiency of an enzyme in the heme synthetic pathway. [Note: Porphyria, derived from the Greek for purple, refers to the red-blue color caused by pigment-like porphyrins in the urine of some patients with defects in heme synthesis.]
1. Clinical manifestations: The porphyrias are classified as erythropoietic or hepatic, depending on whether the enzyme deficiency occurs in the erythropoietic cells of the bone marrow or in the liver. Hepatic porphyrias can be further classified as chronic or acute.
In general, individuals with an enzyme defect prior to the synthesis of the tetrapyrroles manifest abdominal and neuropsychiatric signs, whereas those with enzyme defects leading to the accumulation of tetrapyrrole intermediates show photosensitivity (that is, their skin itches and burns [pruritus] when exposed to sunlight). [Note: Photosensitivity is a result of the oxidation of colorless porphyrinogens to colored porphyrins, which are photosensitizing molecules thought to participate in the formation of superoxide radicals from oxygen. These radicals can oxidatively damage membranes and cause the release of destructive enzymes from lysosomes.]
a. Chronic hepatic porphyria: Porphyria cutanea tarda, the most common porphyria, is a chronic disease of the liver. The disease is associated with severe deficiency of UROD, but clinical expression of the deficiency is influenced by various factors, such as hepatic iron overload, exposure to sunlight, alcohol ingestion, estrogen therapy, and the presence of hepatitis B or C or HIV infections. [Note: Mutations to UROD are found in only 20% of affected individuals. Inheritance is AD.] Clinical onset is typically during the fourth or fifth decade of life. Porphyrin accumulation leads to cutaneous symptoms (Fig. 1) as well as urine that is red to brown in natural light (Fig. 2) and pink to red in fluorescent light.
Figure 1: Skin eruptions in a patient with porphyria cutanea tarda.
Figure 2: Urine from a patient with porphyria cutanea tarda (right) and from a patient with normal porphyrin excretion (left).
b. Acute hepatic porphyrias: Acute hepatic porphyrias (ALA dehydratase–deficiency porphyria, acute intermittent porphyria, hereditary coproporphyria, and variegate porphyria) are characterized by acute attacks of gastrointestinal (GI), neuropsychiatric, and motor symptoms that may be accompanied by photosensitivity (Fig. 3).
Porphyrias leading to accumulation of ALA and PBG, such as acute intermittent porphyria, cause abdominal pain and neuropsychiatric disturbances, ranging from anxiety to delirium. Symptoms of the acute hepatic porphyrias are often precipitated by use of drugs, such as barbiturates and ethanol, which induce the synthesis of the hemecontaining CYP microsomal drug-oxidation system. This further decreases the amount of available heme, which, in turn, promotes increased synthesis of ALAS1.
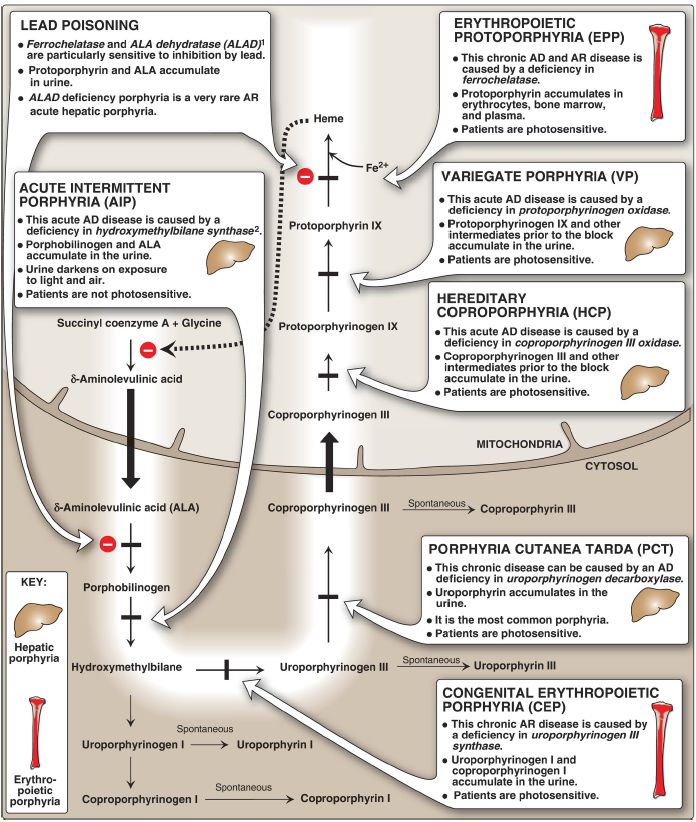
Figure 3: Summary of heme synthesis. 1Also referred to as porphobilinogen synthase. 2Also referred to as porphobilinogen deaminase. [Note: Symptomatic deficiencies in ALA synthase-1 (ALAS1) are unknown. Deficiencies in X-linked ALAS2 result in an anemia.] ALA = δ-aminolevulinic acid; AD = autosomal dominant; AR = autosomal recessive; Fe = iron.
c. Erythropoietic porphyrias: The chronic erythropoietic porphyrias (congenital erythropoietic porphyria and erythropoietic protoporphyria) cause photosensitivity characterized by skin rashes and blisters that appear in early childhood (see Fig. 3).
2. Increased δ-aminolevulinic acid synthase activity: One common feature of the hepatic porphyrias is decreased synthesis of heme. In the liver, heme normally functions as a repressor of the ALAS1 gene. Therefore, the absence of this end product results in an increase in the synthesis of ALAS1 (derepression). This causes an increased synthesis of intermediates that occur prior to the genetic block. The accumulation of these toxic intermediates is the major pathophysiology of the porphyrias.
3. Treatment: During acute porphyria attacks, patients require medical support, particularly treatment for pain and vomiting. The severity of acute symptoms of the porphyrias can be diminished by intravenous injection of hemin and glucose, which decreases the synthesis of ALAS1.
Protection from sunlight, ingestion of β-carotene (provitamin A) that scavenges free radicals, and phlebotomy (removes porphyrins) are helpful in porphyrias with photosensitivity.



|
|
|
|
لخفض ضغط الدم.. دراسة تحدد "تمارين مهمة"
|
|
|
|
|
|
|
طال انتظارها.. ميزة جديدة من "واتساب" تعزز الخصوصية
|
|
|
|
|
|
|
مشاتل الكفيل تزيّن مجمّع أبي الفضل العبّاس (عليه السلام) بالورد استعدادًا لحفل التخرج المركزي
|
|
|