
 النبات
النبات
 الحيوان
الحيوان
 الأحياء المجهرية
الأحياء المجهرية
 علم الأمراض
علم الأمراض
 التقانة الإحيائية
التقانة الإحيائية
 التقنية الحيوية المكروبية
التقنية الحيوية المكروبية
 التقنية الحياتية النانوية
التقنية الحياتية النانوية
 علم الأجنة
علم الأجنة
 الأحياء الجزيئي
الأحياء الجزيئي
 علم وظائف الأعضاء
علم وظائف الأعضاء
 الغدد
الغدد
 المضادات الحيوية
المضادات الحيوية|
Read More
Date: 19-7-2021
Date: 5-11-2015
Date: 15-7-2021
|
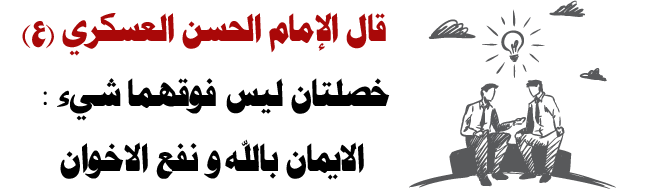
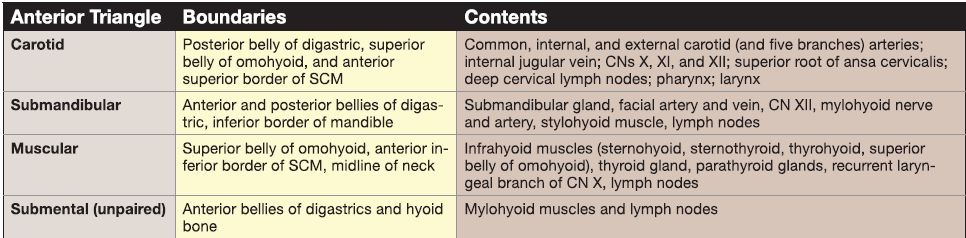
Neck Organization and Contents
The organization of the neck is such that the SCM muscle divides the region into anterior and posterior triangles, bilaterally. The posterior triangle is bound anteriorly by the posterior border of the SCM, posteriorly by the anterior border of the upper trapezius, and inferiorly by the middle third of the clavicle. The anterior triangle is bound posteriorly by the anterior border of the SCM, superiorly by the inferior border of the mandible, anteriorly by the midline of the neck, and inferiorly by the jugular notch of the manubrium. The anterior triangle is further divided by muscular and osseous boundaries to create smaller carotid, submandibular, muscular, and submental triangles (Fig. 1). Contents include the following:
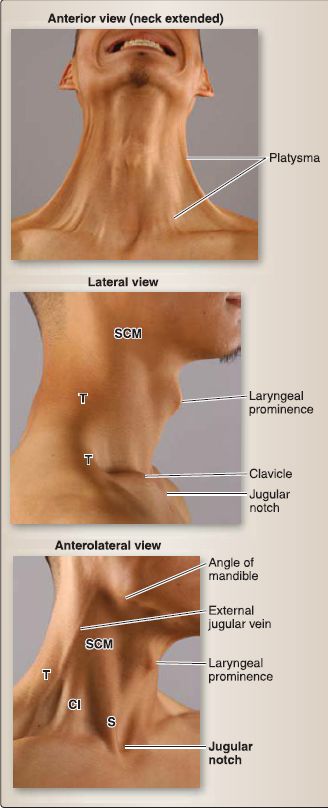
Figure 1: Surface anatomy of neck.
A. Cervical plexus
The cervical plexus is a collection of cervical anterior primary rami (C1-C5) that mediate sensory and motor function in the neck region. Cutaneous branches of the cervical plexus emerge at the nerve point of the neck along the posterior border of the SCM. These branches include the lesser occipital (C2), great auricular (C2-C3), transverse cervical (C2-C3), and supraclavicular nerves (C3-C4). They distribute in the superficial cervical fascia to the scalp, parotid region, anterior neck, and clavicle and superior shoulder region, respectively. Sensory branches that mediate proprioception also distribute to the SCM (C2-C3) and trapezius (C3-C4). Although these muscles receive sensory innervation from branches of the cervical plexus, motor input is provided by the accessory nerve (cranial nerve [CN] IX).
1. Ansa cervicalis: The ansa cervicalis ("loop of the neck"; C1-C3) represents the purely motor component of the cervical plexus. It is partitioned into superior and inferior roots. The C1 superior root component travels a short distance with the hypoglossal nerve (CN XII) before exiting to descend in the carotid triangle of the neck to innervate the infrahyoid muscles in the muscular triangle. The inferior root (C2-C3) loops posteriorly around the internal jugular vein, giving branches to the infrahyoid muscles along its course.
2. Nerves to thyrohyoid and geniohyoid (C1): These nerves also travel with the hypoglossal nerve before exiting to provide motor innervation to these muscles, respectively.
3. Phrenic nerve (C3-C5): This nerve travels inferiorly in the posterior triangle into the thorax to provide motor innervation to the diaphragm and sensory innervation to associated parietal pleura (Fig. 2).
 Figure 2: Cervical plexus. Arrangement and distribution. Orange: somatic motor; light blue: somatic sensory; green: cranial nerve; dark blue: connecting fibers of cervical plexus.
Figure 2: Cervical plexus. Arrangement and distribution. Orange: somatic motor; light blue: somatic sensory; green: cranial nerve; dark blue: connecting fibers of cervical plexus.
B. Musculature
Muscles of the neck can be subdivided into superficial, prevertebral, anterior cervical (suprahyoid and infrahyoid), and visceral (laryngeal and pharyngeal). Many of these muscles serve as boundaries of the triangles of the neck and act on the cervical vertebrae, mandible,hyoid, mouth, larynx, and pharynx. Muscle attachments, action(s),
and innervation are detailed in subsequent sections.
1. Superficial: These muscles include the platysma, SCM, and trapezius (see Fig. 1).
2. Prevertebral: These muscles include the longus colli; longus capitis and rectus capitis (suboccipital triangle musculature); anterior, middle, and posterior scalenes; oblique capitis (suboccipital triangle musculature) and splenius capitis; and levator scapulae.
3. Anterior cervical: Suprahyoid muscles include the digastric (posterior and anterior bellies), mylohyoid, hyoglossus, stylohyoid, and geniohyoid muscles. lnfrahyoid muscles include the sternohyoid, sternothyroid, omohyoid (superior and inferior bellies), and thyrohyoid.
4. Visceral: Laryngeal muscles include the cricothyroid, thyroarytenoid, posterior and lateral cricoarytenoid, vocalis, and transverse and oblique arytenoid muscles. Pharyngeal muscles include the constrictors (superior, middle, and inferior), palatopharyngeus, stylopharyngeus, and salpingopharyngeus.
C. Vasculature and lymphatics
The neck receives a rich blood supply from the carotid system, which also contributes to blood supply of the head. Venous drainage occurs through tributaries of the jugular system. Lymphatic channels follow the veins and drain through a subset of cervical and visceral nodes.
1. Arterial supply: Arterial supply to the neck is supplied by branches of the external carotid and subclavian arteries. In the neck, the right and left common carotid arteries travel in the carotid sheath and bifurcate at the superior boundary of the thyroid cartilage into
external and internal carotid arteries. The carotid body and carotid sinus are located at the level of bifurcation. The internal carotid artery continues unbranched toward the head, whereas the external gives off a series of branches in the neck. The subclavian artery, a branch of the brachiocephalic trunk on the right and a direct branch of the aortic arch on the left, travels through the posterior triangle of the neck on way to the upper limb, giving off important branches along its course. It is divided into three parts by the anterior scalene muscle (Fig. 3).
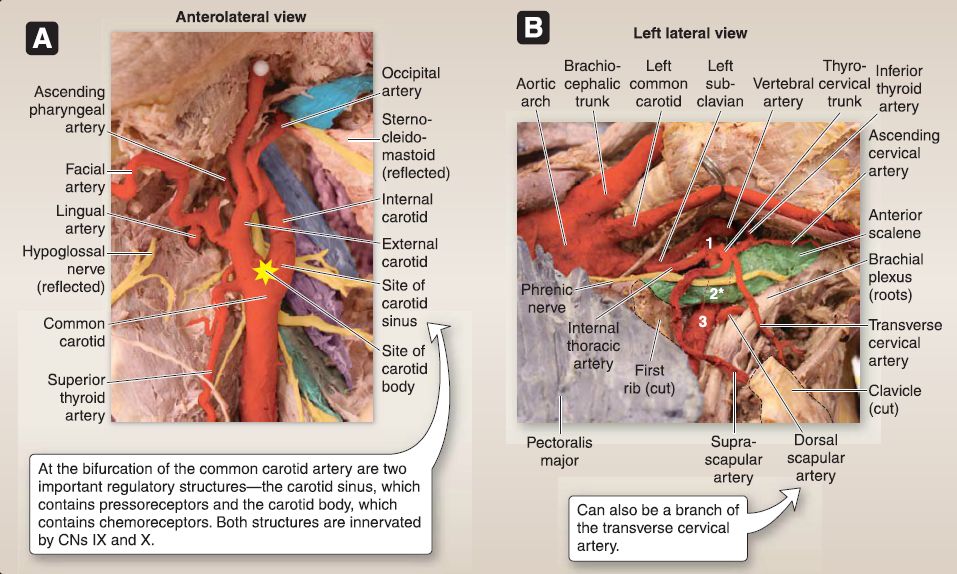 Figure 3: Vasculature of the neck. A, Carotid system in the neck (image rotated to illustrate anatomy in the standing position). B, Subclavian artery and branches (supine). *costocervical trunk branches from second part of subclavian artery Note that the internal jugular vein has been removed. CN = cranial nerve.
Figure 3: Vasculature of the neck. A, Carotid system in the neck (image rotated to illustrate anatomy in the standing position). B, Subclavian artery and branches (supine). *costocervical trunk branches from second part of subclavian artery Note that the internal jugular vein has been removed. CN = cranial nerve.
a. External carotid: The external carotid artery gives off branches originating in the carotid triangle of the neck, including the superior thyroid (which, in turn, gives off the superior laryngeal branch), lingual, facial, ascending pharyngeal, and occipital branches, as well as posterior auricular, maxillary, and superficial temporal branches (Fig. 4).
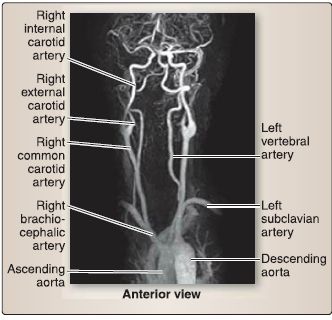
Figure 4: Angiograph of neck arteries.
b. Subclavian: Part one gives off vertebral, internal thoracic, thyrocervical trunk (which, in turn, gives off inferior thyroid, transverse cervical, and suprascapular branches). Part two gives off the costocervical trunk (which, in turn, gives off the deep cervical branch). Part three gives off the dorsal scapular branch (which can also arise from the transverse cervical artery).
2. Venous drainage: Venous drainage occurs primarily by way of internal jugular and subclavian vein tributaries. A series of superficial venous structures, including the external jugular, anterior jugular, and communicating branch veins, also contribute to drainage of neck structures (Fig. 5).
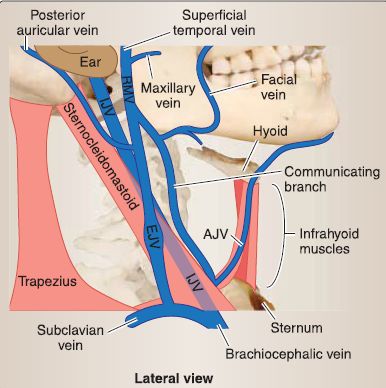
Figure 5: Venous network in the neck.AJV = anterior jugular vein, EJV = external jugular vein, IJV = internal jugular vein, RMV = retromandibular vein.
a. Internal jugular: This vein is continuous with the sigmoid sinus (dural) in the skull and joins the subclavian vein to form the brachiocephalic vein.
b. External jugular: This vein lies anterior to the SCM and is formed by converging retromandibular and posterior auricular veins.
3. Lymphatics: Lymphatic vessels in the neck generally follow the veins. Superficial cervical lymph nodes are located along the course of the external jugular vein and drain lymph from superficial neck structures into deep cervical nodes. The primary chain of deep cervical nodes is associated with the internal jugular vein, deep to the SCM muscle. Deep cervical node efferent vessels converge to form the right and left jugular lymphatic trunks, which drain into the right venous angle and thoracic duct, respectively. Several subgroups of lymph nodes are associated with specific neck structures (Fig. 6).
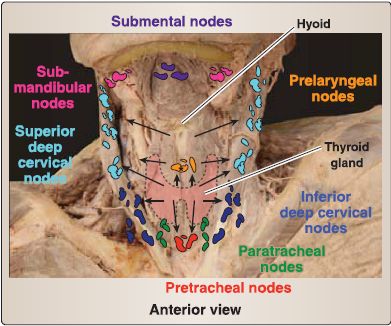
Figure 6: Lymphatic system in the neck. Black arrows indicate direciton of lymph flow.
D. Triangles
As previously described, the right and left sides of the neck are divided into posterior and anterior triangles by the SCM muscle (Fig. 7). The SCM originates from the mastoid process and superior nuchal line laterally and inserts onto the manubrium and medial clavicle. Acting unilaterally, it side-bends the neck to the same side and rotates opposite. Acting bilaterally, it flexes the neck and extends the atlanto-occipital joints. It receives motor innervation by the accessory nerve (CN XI) and proprioceptive and pain innervation by C2-C3 anterior primary rami.
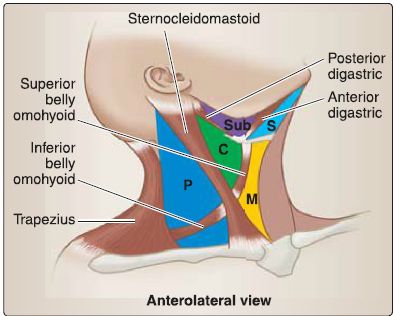
Figure 7: Triangles of the neck. Schematic representation of the muscular boundaries. P = posterior triangle, anterior triangle, C = carotid, M = muscular, S = submental, Sub = submandibular.
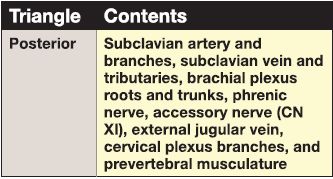
1. Posterior triangle: The posterior triangle contains important muscular and neurovascular structures that function within the neck as well as travel to the upper limb and thorax (Figs. 8 and 9; Table 1). Muscles contribute to the floor of the posterior triangle in addition to acting on the head and neck.
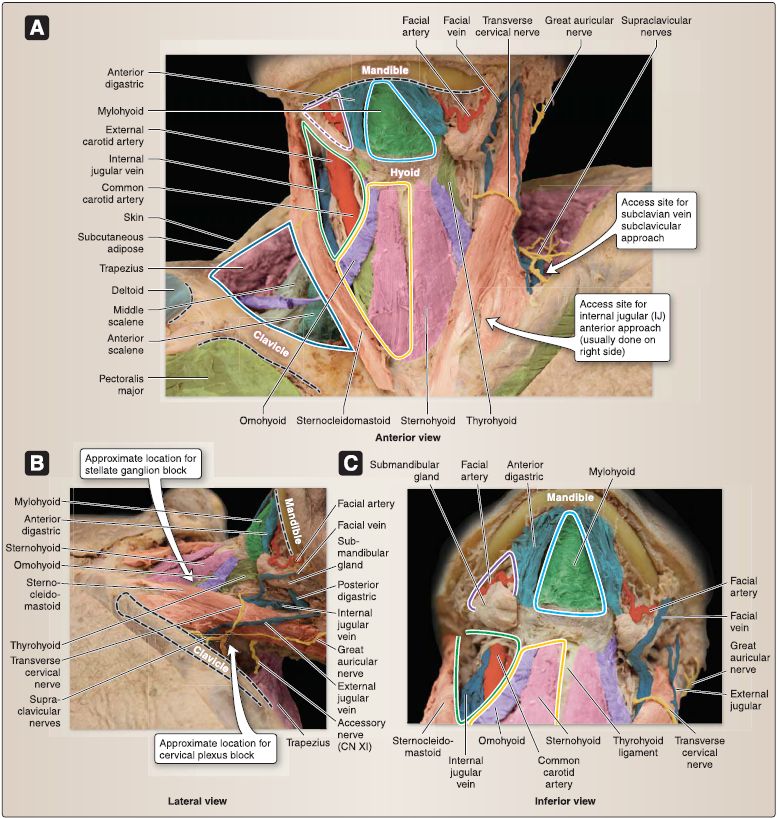
Figure 8: Dissection showing anterior and posterior triangles and associated structures. A, Paired (right side only) and unpaired triangles are outlined. B, Cervical plexus (supine). C, Relationship of anterior neck triangles. Blue = posterior triangle. Anterior triangle: Green = carotid, Yellow = muscular, Violet = submandibular, Aqua = submental.
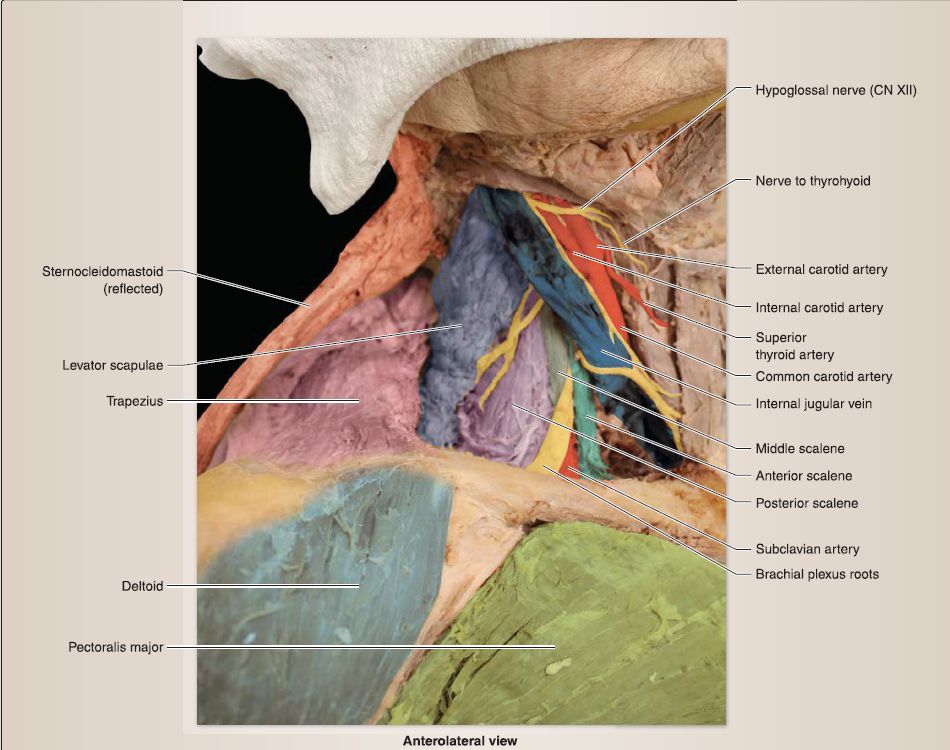 Figure 9: Posterior triangle: root of neck.
Figure 9: Posterior triangle: root of neck.
Table 1: Contents of the Posterior Triangle
a. Scalenes: Common actions of these muscles include neck flexion and associated rib elevation during forced inspiration. Innervation is from cervical anterior primary rami.[1] Anterior: The anterior scalene originates on C3-C6 transverse processes (anterior tubercles) and inserts onto the first rib. The anterior scalene muscle serves as an important landmark in the posterior triangle. The subclavian vein, phrenic nerve, and transverse cervical and suprascapular vessels lie anterior to the anterior scalene. The subclavian artery, costocervical trunk, and brachia! plexus roots/trunks lie posterior to the anterior scalene (see Fig. 9).
[2] Middle: The middle scalene originates on C4-C7 transverse processes (posterior tubercles) and inserts onto the first rib.
[3] Posterior: The posterior scalene originates on C4-C6 transverse processes (posterior tubercles) and inserts onto the second rib.
b. Splenius capitis: This muscle originates from the inferior portion of the nuchal ligament and T1-T6 spinous processes and inserts onto the mastoid process and superior nuchal line.
[1] Actions: Unilaterally, it side-bends and rotates the head to the same side. Bilaterally, it extends the head and neck.
[2] Innervation: It is innervated by segmental posterior primary cervical rami.
c. Longus colli: This muscle originates from the C1 anterior tubercle, C2-C3 vertebral bodies, and C3-C6 transverse processes and inserts onto CS-T3 vertebral bodies and C3-C5 transverse processes.
[1] Actions: Longus colli flexes and side-bends the neck.
[2] Innervation: It is innervated by C2-C6 anterior primary rami.
d. Longus capitis: This muscle originates from the basilar occipital
bone and inserts onto C3-C6 transverse processes (anterior
tubercle).
[1] Actions: Longus capitis flexes the head on the neck at
atlanto-occipital joints.
[2] Innervation: It is innervated by C1-C3 anterior primary rami.
2. Anterior triangle: The anterior triangle is further divided by muscular and osseous boundaries (Table 2). Subdivisions include carotid, submandibular, muscular, and submental triangles.
Table 2: Boundaries and Contents of the Anterior Triangle
a. Carotid triangle: The carotid triangle serves as a passageway for the following important neurovascular structures.
[1] External carotid artery: Five of the eight branches of the external carotid artery branch within the carotid triangle to reach the following structures in the head and neck (Fig. 10).
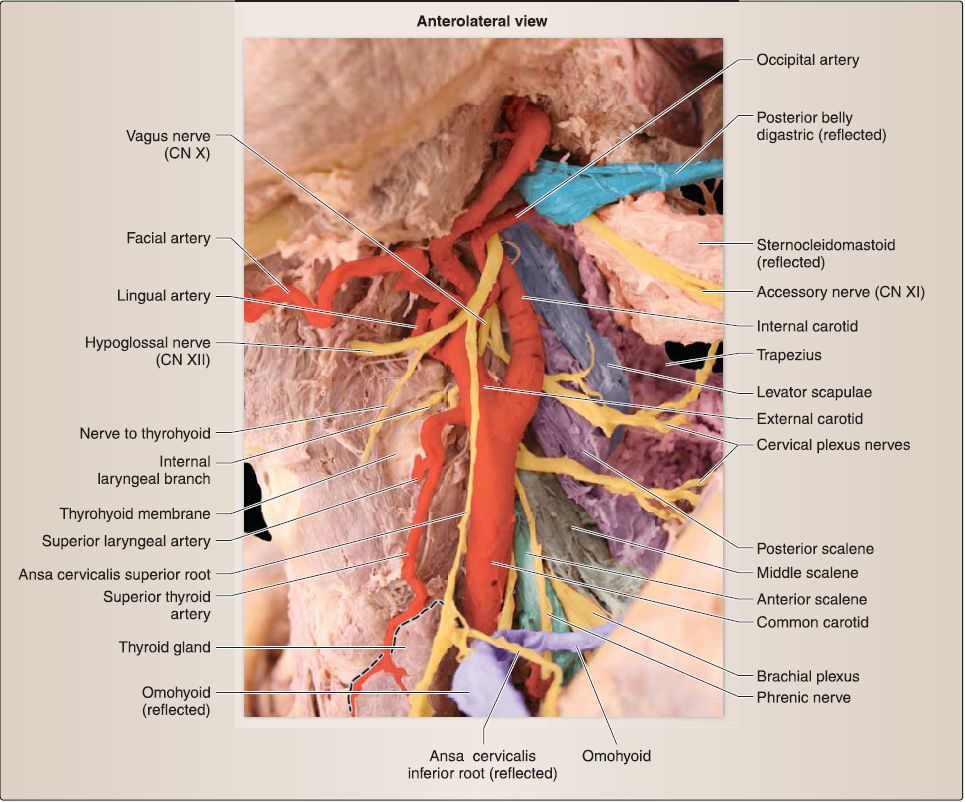 Figure 10: Branches of the external carotid artery and surrounding structures in the carotid triangle. Note that the submandibular gland and internal jugular vein have been removed.
Figure 10: Branches of the external carotid artery and surrounding structures in the carotid triangle. Note that the submandibular gland and internal jugular vein have been removed.
(a} Superior thyroid: This branch serves the thyroid gland. It gives off the superior laryngeal artery that pierces the thyrohyoid membrane to enter the larynx.
(b) Lingual: This branch serves the oral cavity.
(c) Facial: Tortuous in nature, this branch serves the face. It is associated with the submandibular gland and branches in the face.
(d} Ascending pharyngeal: This small vessel branches just superior to the carotid bifurcation and travels superomedially to serve the pharynx.
(e) Occipital: This branch serves the scalp in the occipital region.
[2] Internal jugular: This vein is located lateral to the carotid vessels. The ansa cervicalis typically loops around the internal jugular vein.
[3] Vagus nerve: CN X descends in the neck posterior to and between the internal jugular and carotid vessels within the carotid sheath. Along its course, the vagus nerve gives off a superior laryngeal branch, which splits into internal laryngeal and external laryngeal nerves. These branches either pierce the thyrohyoid membrane to mediate sensation to the laryngeal mucosa above the vocal folds or travel to the cricothyroid muscle to provide branchiomotor innervation, respectively.
[4] Cervical sympathetic trunk: Located at the same depth as the vagus nerve, the cervical sympathetic trunk lies medial to the contents of the carotid sheath (Fig. 11).
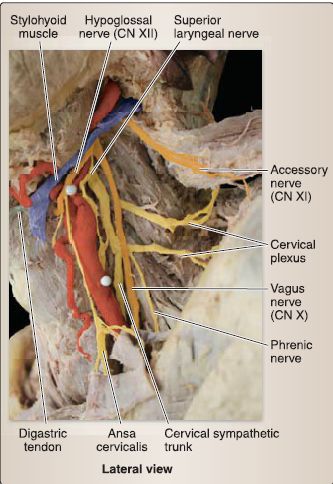
Figure 11: Orientation of cervical sympathetic trunk and vagus nerve. Note that the cranial nerves are shown in orange color and internal jugular vein has been removed.
[5] Accessory nerve: CN XI exits the skull and passes through the carotid triangle on its way to the SCM and trapezius muscles.
[6] Hypoglossal nerve: CN XII travels through the carotid triangle on its way to the oral cavity. Branches of the cervical plexus run with the hypoglossal nerve and exit within the triangle as the superior root of the ansa cervicalis and the nerves to thyrohyoid and geniohyoid (C1).
b. Submandibular triangle: Bound by the digastric muscle bellies and inferior mandible, the submandibular triangle is primarily occupied by the superficial portion of the submandibular gland. Facial vessels travel adjacent to the gland to reach the face .
[1] Digastric muscle: The digastric muscle is made up of two bellies-anterior and posterior-which originate from the digastric fossa of the mandible and mastoid process, respectively. An intermediate tendon serves as a common insertion site, which is attached to the body and greater horn of the hyoid bone. The anterior belly receives branchiomotor innervation from the trigeminal nerve (CN V3; nerve to mylohyoid), whereas the posterior belly receives branchiomotor innervation from the facial nerve (CN VII). Collectively, the digastric muscle assists in steadying the hyoid bone during swallowing and speech and also depresses the mandible against resistance.
[2] Hypoglossal nerve: CN XII passes posterior to the posterior belly of the digastric muscle to enter the triangle and continue to the oral cavity.
[3] Stylohyoid muscle: Also associated with the posterior belly of the digastric muscle is the stylohyoid, which arises from the styloid process and sends muscle fibers on either side of the common digastric tendon to insert onto the hyoid bone. The stylohyoid is innervated by the facial nerve (CNVII) and assists the digastric muscles in elevating the hyoid bone during swallowing.
[4] Nerve and artery to mylohyoid: Finally, these emerge deep to the mandible to reach the mylohyoid muscle through the submandibular triangle.
c. Muscular triangle: The muscular triangle contains the infrahyoid muscles and underlying neck viscera (Fig. 12).
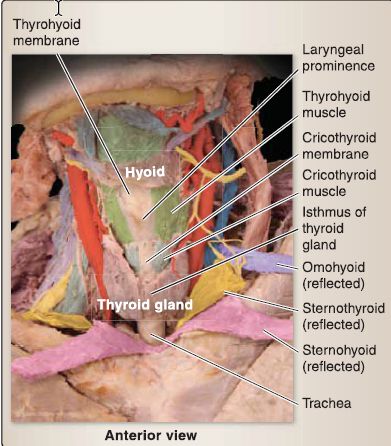
Figure 12: Anterior neck, muscular triangle (deep structures).
[1] lnfrahyoid muscles: The infrahyoid muscles receive motor innervation from the ansa cervicalis primarily. The exception to this is the thyrohyoid, which receives the nerve to thyrohyoid (C1) directly. Collectively, the infrahyoid musclessternohyoid, sternothyroid, thyrohyoid, and omohyoid (omo = scapula)-attach to the structures in their names.
The omohyoid has superior and inferior bellies, which serve as muscular borders in the neck. lnfrahyoid muscles play an important role in swallowing and phonation. Specific functions include:
(a) Sternohyoid: This muscle depresses the hyoid bone from an elevated position during swallowing.
(b) Sternothyroid: This muscle depresses the hyoid bone and larynx.
(c) Thyrohyoid: This muscle depresses the hyoid bone and elevates the larynx.
(d) Omohyoid: This muscle depresses, steadies, and retracts the hyoid bone.
[2] Thyroid gland: The butterfly-shaped bi lobar thyroid gland is found in the muscular triangle just inferior to the thyroid cartilage. The right and left lobes of the thyroid are connected anteriorly by an isthmus at approximately the second or third tracheal ring level.
[3] Parathyroid glands: These are typically located bilaterally on the posterior surface of the thyroid gland.
[4] Recurrent laryngeal nerve: This branch of the vagus nerve (CN X) courses in the muscular triangle in a groove between the trachea and esophagus, deep and lateral to the thyroid gland. It eventually courses into the larynx to mediate sensation to the mucosa below the vocal folds as well as to provide branchiomotor innervation to the remaining intrinsic laryngeal muscles. The recurrent laryngeal nerve is also referred to as the inferior laryngeal nerve once it enters the larynx.
d. Submental triangle: This unpaired triangle is bound by the anterior bellies of the digastric muscles laterally and the hyoid bone inferiorly . The mylohyoid muscle, which originates from the mylohyoid line of the mandible and inserts along a midline raphe and hyoid bone, forms the floor of the triangle. The mylohyoid receives branchiomotor innervation from the trigeminal nerve (CN V3) and assists in swallowing and phonation by elevating the hyoid bone, tongue, and floor of the oral cavity. Submental lymph nodes lie superficial to the mylohyoid muscle within the boundaries of the triangle.



|
|
|
|
علامات بسيطة في جسدك قد تنذر بمرض "قاتل"
|
|
|
|
|
|
|
أول صور ثلاثية الأبعاد للغدة الزعترية البشرية
|
|
|
|
|
|
|
مكتبة أمّ البنين النسويّة تصدر العدد 212 من مجلّة رياض الزهراء (عليها السلام)
|
|
|