


 النبات
النبات
 الحيوان
الحيوان
 الأحياء المجهرية
الأحياء المجهرية
 علم الأمراض
علم الأمراض
 التقانة الإحيائية
التقانة الإحيائية
 التقنية الحيوية المكروبية
التقنية الحيوية المكروبية
 التقنية الحياتية النانوية
التقنية الحياتية النانوية
 علم الأجنة
علم الأجنة
 الأحياء الجزيئي
الأحياء الجزيئي
 علم وظائف الأعضاء
علم وظائف الأعضاء
 الغدد
الغدد
 المضادات الحيوية
المضادات الحيوية|
Read More
Date: 18-7-2021
Date: 10-7-2021
Date: 21-7-2021
|
Perineum
The perineum represents the region inferior to the pelvic diaphragm and is associated with male and female external genitalia and the anus (Fig. 1). It is a diamond-shaped area that is further divided into an anterior urogenital triangle and a posterior anal triangle. The triangles share a common boundary represented by an imaginary line drawn between the right and left ischial tuberosities. Here, the development and anatomy of the female and male perineum is presented. The remaining structures of the female and male reproductive systems are presented with pelvic viscera.

Figure 1: Perineum. Urogenital and anal triangle boundaries.
A. Urogenital triangle
Bound by the ischiopubic rami, pubic symphysis, and an imaginary line drawn through the ischial tuberosities, the urogenital triangle is described as having superficial and deep perinea! spaces (pouches). Homologous female and male structures are organized into either the superficial or deep space.
1. External genitalia development: Starting in week 5, a proliferationof mesoderm around the cloacal membrane causes the overlying ectoderm to rise up so that three structures are visible externally: the phallus, urogenital folds, and labioscrotal swellings. These primordia continue to develop and differentiate into homologous structures in both sexes.
a. Female: As shown in Figure 2, the phallus in the female forms the clitoris (glans clitoris, corpora cavernosa clitoris, and vestibular bulbs). The urogenital folds in the female form the labia minora. The labioscrotal swellings in the female form the labia majora and mons pubis.
b. Male: As shown in Figure 3, the phallus in the male forms the penis (glans penis, corpora cavernosa penis, and corpus spongiosum penis). The urogenital folds in the male fuse in the midline and form the ventral aspect of the penis and penile raphe. The labioscrotal swellings in the male fuse in the midline and form the scrotum and scrotal raphe.
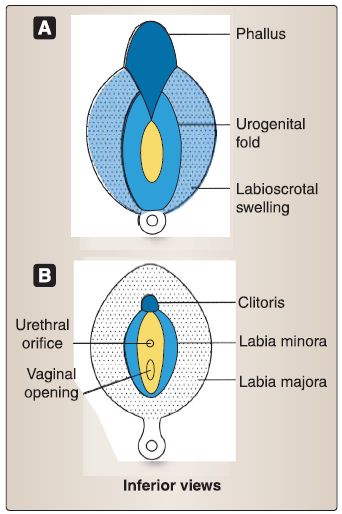
Figure 2:A and B, Female external genitalia embryology.

Figure 3: A and B, Male genitalia embryology.
2. Urogenital triangle anatomy: Differentiation of male and female primordial structures in the urogenital triangle results in fusion of bilateral structures in the male and maintenance of bilateral structures with a midline cleft-vestibule-in the female. Table .1 lists homologous perineal structures in the adult female and male.
Table1: Homologous Perineal Structures

Structures in the male and female urogenital triangle are described as being in the superficial perinea pouch or space, as they are suspended from a broad sheet of fascia-perinea! membrane. The perinea! membrane spans the width of the urogenital triangle, serving as the superior and inferior boundaries of the superficial and deep perinea! pouches, respectively. Erectile tissues in both the female and male external genitals are cavernous by design, allowing for vasocongestion during sexual arousal and erection. Surrounding musculature contracts to maintain erection by limiting venous drainage.
a. Female: Structures of the female urogenital triangle include bilateral labia majora and minora, a midline superior mons pubis, clitoris, and vestibule of the vagina. Female external genitalia collectively make up the vulva .
[1] Labia majora: Labia majora are hair-covered longitudinal folds with varying degrees of fat on either side of the vestibule.
[2] Labia minora: Labia minora are hairless, thin longitudinal folds found medial and deep to labia majora, and also frame the vestibule. Anteriorly, the labia minora contribute skin to form the prepuce and frenulum of the clitoris.
[3] Clitoris: The clitoris is nestled between the prepuce and frenulum and consists of a body and glans, which are formed by specialized erectile tissue. Proximally, the body is formed by bilateral corpora cavernosa and a commissure of the bulbs. Distally, the commissure of the bulbs expands to form the glans clitoris. Posteriorly, the corpora cavernosa and commissure of the bulbs expand to form the crura of the clitoris and the vestibular bulbs, respectively.
[4] Vestibule: The vestibule of the vagina is located between the labia minora and contains the external urethral orifice and the vaginal opening. Paraurethral, greater vestibular, and lesser vestibular glands open into this space.
[5] Female perineal muscles: Female perineal muscles include ischiocavernosus and bulbospongiosus, which cover the crura of the clitoris and vestibular bulbs, respectively (Fig. 4 ). These muscles function to keep blood in the erectile tissues and maintain clitoral erection. Bulbospongiosus also compresses the greater vestibular gland and attaches at the perinea! body, thereby strengthening the structure. Superficial transverse perineal muscles course across the posterior border of the urogenital triangle, also inserting into and supporting the perineal body.
 Figure 4:Muscles of the female perineum. Cadaveric (left; adductors intact) and schematic (right; adductors removed) representation of female urogenital triangle structures. PM = perineal membrane.
Figure 4:Muscles of the female perineum. Cadaveric (left; adductors intact) and schematic (right; adductors removed) representation of female urogenital triangle structures. PM = perineal membrane.
b. Male: Structures of the male urogenital triangle include the scrotum and penis . A major distinction in the male urogenital triangle is the lack of a midline cleft, as is seen in the female. During development, male structures fuse along the midline, which is evident by a scrotal and penile raphe.
[1] Scrotum: The scrotum is a hair-covered outpouching of the anterior abdominal wall and is, therefore, made up of cutaneous and fascial layers. The superficial perineal fascia is deep to the skin and is the perineal continuation of the superficial fascia of the abdomen. Within the fascia lays a layer of smooth muscle-dartos muscle-which functions primarily when the scrotum is exposed to cold temperatures.
The scrotum contains a portion of the spermatic cord and the testes .
[2] Penis: The penis is rooted at its base and extends distally as into a hairless mobile body (shaft). It is formed by paired corpora cavernosa and an unpaired corpus spongiosum. These cylinders of erectile tissue have a sponge-like appearance on cross section, which is interrupted centrally by the deep arteries of the penis and the spongy urethra in the corpora cavernosa and corpus spongiosum, respectively.
Paired corpora cavernosa in the penile shaft separate into right and left crura, which anchor the penis to the ischiopubic rami. The corpus spongiosum expands proximally into the bulb of the penis (base), which anchors the penis to the perineal membrane. It expands distally into the glans penis, which is covered by a double layer of skin, the prepuce (foreskin) in an uncircumcised individual. The penis is supported by facial layers, including the tunica albuginea around each cylinder and the deep fascia of the penis around all three cylinders. Neurovascular bundles travel between fascial layers. A thin layer of loose areolar tissue (superficial perineal fascia) separates the deep fascia from the overlying skin.
[3] Male perinea! muscles: This group of muscles includes ischiocavernosus and bulbospongiosus, which cover the crura and bulb of the penis, respectively (Fig. 5). These muscles function to keep blood in the erectile tissues and maintain clitoral erection. Bulbospongiosus also compresses the bulb of the penis to expel urine and ejaculate and attaches at the perineal body, thereby strengthening the structure.
 Figure 5:Muscles of the male perineum. Cadaveric (left; adductors intact) and schematic (right; adductors removed) representation of male urogenital triangle structures.
Figure 5:Muscles of the male perineum. Cadaveric (left; adductors intact) and schematic (right; adductors removed) representation of male urogenital triangle structures.
Superficial transverse perinea! muscles course across the posterior border of the urogenital triangle, also inserting into and supporting the perineal body.
c. Perinea! vasculature: Genital structures of the perineum rely on adequate blood supply for erectile tissue engorgement (Fig. 6). Coordination between vasculature and perinea! musculature is necessary during clitoral/penile erection and remission.
 Figure 6:Neurovascular supply of perineum. A, Female. B, Male. PS = pubic symphysis.
Figure 6:Neurovascular supply of perineum. A, Female. B, Male. PS = pubic symphysis.
[1] Arterial supply: The internal pudendal artery is the primary arterial supply to the male and female perineum. A branch of the internal iliac (anterior division), the internal pudendal artery courses through the greater and lesser sciatic foramina, travels through the pudendal canal, and gives off inferior rectal arteries in the ischioanal fossa. It continues as the perineal artery and gives off branches to the labia/ scrotum and bulb of the vestibule/penis before terminating into deep and dorsal arteries of the clitoris/penis.
[2] Venous drainage: Venous drainage occurs partially through branches of internal and external pudendal veins. Venous blood in the corpora cavernosa is drained through the deep dorsal vein of the clitoris/penis, which is a tributary of the vesicle/prostatic venous plexus.
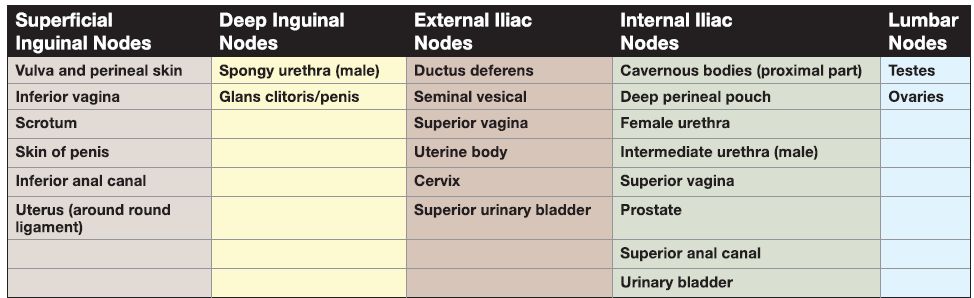
d. Lymphatics: Lymphatic drainage of perineal structures occurs through either superficial inguinal or internal iliac lymph nodes. Table .2 lists the lymphatic drainage of the pelvis and
perineum.
Table .2: Perineal Lymphatics
e. Innervation: The perineum is rich with innervation, as it is a highly sensitive area. While primary innervation is provided through the pudenda! nerve (somatic), reproductive function of perinea! structures also requires autonomic control .
[1] Somatic innervation: Somatic innervation to the perineum occurs through the pudendal nerve (S2-S4). Like the internal pudenda! vessels, the pudenda! nerve exits the pelvis through the greater sciatic foramen and reenters the perineum through the lesser sciatic foramen. After giving off inferior rectal nerves in the ischioanal fossa, the nerve continues as the perinea! nerve, which then divides into superficial and deep branches. Superficial branches supply the scrotum/posterior vulva. Deep branches innervate the muscles of the perineum and receive sensory input from erectile tissue of the vestibular bulb/bulbospongiosum. The deep branches continue as the dorsal nerve of the clitoris/penis and travel through the deep perinea! pouch along the ischiopubic ramus to emerge on the dorsal surface of the clitoris/penis and provide sensory innervation. Additional sensory innervation to this region is provided by branches of the ilioinguinal, genitofemoral, and posterior femoral cutaneous nerves. [2] Autonomic innervation: Autonomic sympathetic fibers primarily distribute with branches of the pudenda! nerve . Pelvic splanchnic nerves (S2-S4) contribute to the vesicle/prostatic plexuses, which give rise to cavernous nerves. These parasympathetic fibers distribute to microvasculature of erectile bodies (clitoris/penis) and are responsible for engorgement/erection of the clitoris/penis.
B. Anal triangle
Bound by the sacrotuberous ligaments bilaterally, coccyx posteriorly, and an imaginary line drawn through the ischial tuberosities, the anal triangle houses the centrally located anal canal and anus, bound by fat-laden ischioanal fossae bilaterally . As the distal end of the GI tract terminates in this region, development of the anal canal is detailed here before describing anatomy in the anal triangle.
1. Embryologic formation of the anal canal: As shown in Figure 7, the upper anal canal develops from the hindgut. The lower anal canal develops from the proctodeum, which is an invagination of surface ectoderm caused by a proliferation of mesoderm surrounding the anal membrane. The dual components (hindgut and proctodeum) involved in the embryologic formation of the entire anal canal determine the gross anatomy of this area, which becomes important when considering the clinical characteristics of hemorrhoids and metastasis of anorectal tumors. The junction between the upper and lower anal canals is indicated by the pectinate line in the adult, which also marks the site of the former anal membrane.

Figure 7:A-D, Embryologic formation of the anal canal, A-C Embryologic formation of
the anal canal. A, week 4, B, week 6, C, week 8, D, Photograph of adult anal canal.
2. Anal canal anatomy: The anal canal makes up the distal 2 inches of the GI tract. It is continuous with the rectum at the anorectal junction and extends to the anus. The upper anal canal is characterized by longitudinal mucosal ridges called anal columns, which are connected inferiorly by anal valves. The inferior border of the valves forms the pectinate line and demarcates upper from lower anal canals and, in turn, a transition of neurovascular and lymphatic supply (Fig. 8).
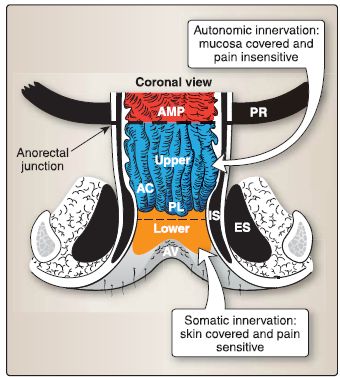
Figure 8: Schematic of anal canal. AC = anal column, AMP = ampulla of rectum, AV = anal verge, ES = external anal sphincter, IS = internal anal sphincter, PL = pectinate line, PR = puborectalis muscle.
a. Muscles: The anal canal is supported by both smooth and skeletal sphincters. The internal (involuntary) anal sphincter surrounds the upper anal canal and extends inferiorly to lie medial to the external (voluntary) anal sphincter. The external anal sphincter has three parts-deep, superficial, and subcutaneous-and contributes to the formation of the perineal body.
b. Blood supply: As shown in Figure 9, superior to the pectinate line, the upper anal canal is supplied by the superior rectal artery from inferior mesenteric artery (abdominal aorta). Venous drainage occurs through the rectal plexus into superior rectal vein of the portal system. Inferior to the pectinate line, the lower anal canal is supplied by the inferior rectal arteries from internal pudenda! artery (internal iliac). Venous drainage occurs through inferior rectal veins, ultimately draining into the caval system. The anal canal is an important site for portacaval anastomoses.
c. Innervation: Superior to the pectinate line, the upper anal canal structures receive autonomic fibers through the rectal plexus, which is continuous with the inferior hypogastric plexus . Inferior to the pectinate line, the lower anal canal structures receive somatic innervation from the inferior rectal nerves, branches of the pudenda! nerve. Fecal continence involves the coordination of both internal and external anal sphincters and the puborectalis muscle. Sympathetic stimulation causes tonic contraction of internal anal sphincter, while parasympathetic stimulation causes relaxation.
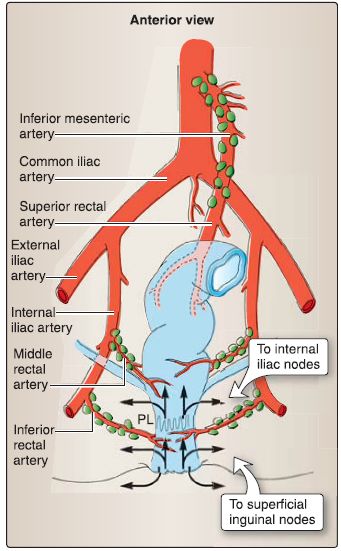
Figure 9:Anal canal arterial supply and lymphatics. PL = pectinate line.
d. Lymphatics: Upper anal canal structures drain to internal iliac nodes, while lower anal structures drain to superficial inguinal nodes .
3. Anal canal histology: As previously stated, the anal canal is divided into the upper and lower anal canals by the pectinate line (Fig. 10). The anal canal ends at the anal verge where the
perianal skin begins.
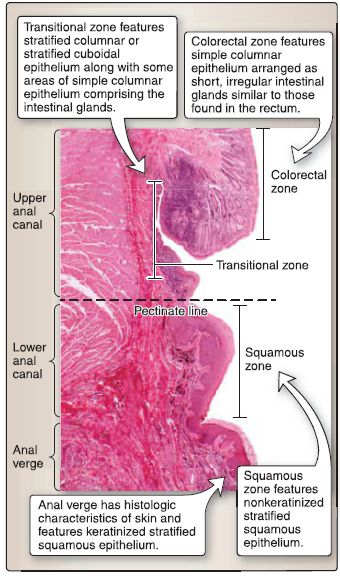
Figure 5.18:Anal canal histology.
a. Upper anal canal: The wall of the upper anal canal consists of four histologic layers: mucosa, submucosa, muscularis externa, and adventitia.
[1] Mucosa: The mucosa and the submucosa of the upper anal canal extend into longitudinal folds called the anal columns (or columns of Morgagni). The base of the anal columns defines the pectinate line. The anal columns are connected at their bases by transverse folds of mucosa called the anal valves. Behind the anal valves are small, blind pouches called the anal sinuses into which mucous anal glands open. The mucosa of the upper anal canal consists of an epithelium, lamina propria, and muscularis mucosa. The mucosaof the upper anal canal is characterized by the colorectal zone and the transitional zone as defined by the type of epithelium present. The lamina propria consists of loose connective tissue, blood vessels, and diffuse lymphatic tissue. The muscularis mucosa consists of a smooth muscle layer that may not be prominent.
(a) Colorectal zone: Immediately distal to the rectum, the colorectal zone features simple columnar epithelium arranged as short, irregular intestinal glands similar to those found in the rectum.
(b} Transitional zone: The transitional zone features a transition from simple columnar epithelium to stratified columnar epithelium or stratified cuboidal epithelium, along with some areas of simple columnar epithelium comprising the intestinal glands.
[2] Submucosa: The submucosa of the upper anal canal consists of dense, irregular connective tissue; blood vessels, in particular the superior hemorrhoidal venous plexus; anal glands that open into the anus sinuses; diffuse lymphatic tissue; and the submucosal (Meissner) nerve plexus. The mucosa and the submucosa of the upper anal canal extend into anal columns.
[3] Muscularis externa: The muscularis externa of the upper anal canal consists of an inner circular layer of smooth muscle that thickens to form the internal anal sphincter, an outer longitudinal layer of smooth muscle (may not be prominent), and the myenteric (Auerbach) nerve plexus.
[4] Adventitia: The adventitia of the upper anal canal consists of dense, irregular connective tissue that blends in with the connective tissue of the body wall.
b. Lower anal canal: The wall of the lower anal canal also consists of mucosa, submucosa, muscularis externa, and adventitia.
[1] Mucosa: The mucosa of the lower anal canal consists of an epithelium, lamina propria, and muscularis mucosa. The mucosa of the lower anal canal is characterized by a squamous zone as defined by the type of epithelium present. Located immediately distal to the pectinate line, the squamous zone features nonkeratinized stratified squamous epithelium. The lamina propria consists of loose connective tissue, blood vessels, and diffuse lymphatic tissue. The muscularis mucosa consists of a smooth muscle layer, which may not be prominent.
[2] Submucosa: The submucosa of the lower anal canal consists of dense, irregular connective tissue; blood vessels, in particular the inferior hemorrhoidal venous plexus; diffuse lymphatic tissue; and the submucosal (Meissner) nerve plexus.
[3] Muscularis externa: The muscularis externa of the lower anal canal consists of an inner circular layer of smooth muscle that thickens to form the internal anal sphincter, an outer layer of skeletal muscle called the external anal sphincter, and the myenteric (Auerbach) nerve plexus.
[4] Adventitia: The adventitia of the upper anal canal consists of dense, irregular connective tissue that blends in with the connective tissue of the body wall.
c. Anal verge: The anal verge has the histologic characteristics of skin (not the GI tract), which consists of the epidermis and dermis. The epidermis of the anal verge features keratinized stratified squamous epithelium. The dermis consists of dense, irregular connective tissue, blood vessels, lymphatics, myelinated and unmyelinated axons, sensory receptors, hair follicles with sebaceous glands, and circumanal glands (apocrine sweat glands).
4. lschioanal fossae: lschioanal fossae are wedge-shaped, fat-laden spaces located on either side of the anal canal (Fig. 11).
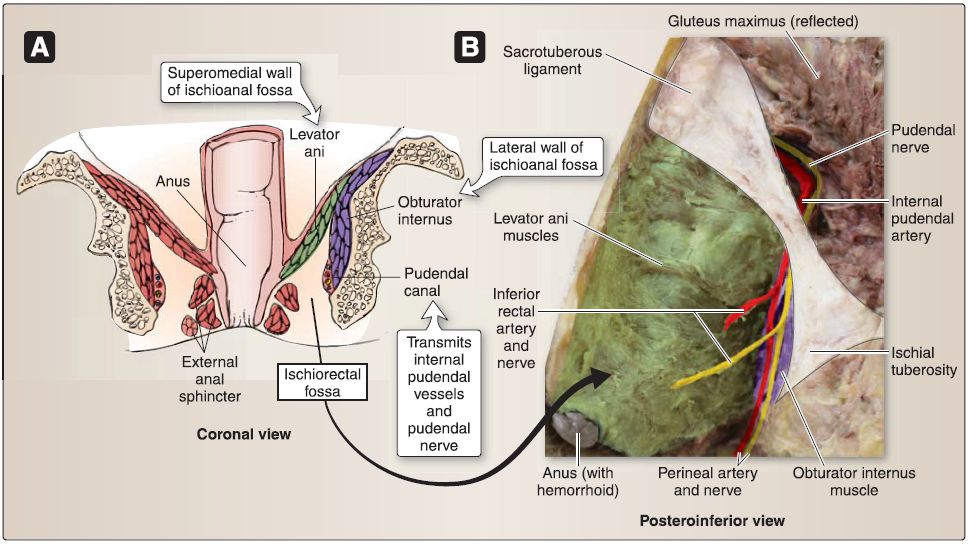 Figure 11: lschioanal fossa. A, Schematic showing boundaries of ischioanal fossa. B, Cadaveric specimen with neuromuscular bundle released from pudendal canal.
Figure 11: lschioanal fossa. A, Schematic showing boundaries of ischioanal fossa. B, Cadaveric specimen with neuromuscular bundle released from pudendal canal.
a. Boundaries: Each space is bound by the levator ani muscles and anal canal medially, obturator internus muscle and ischial tuberosity laterally, and skin and fascia of the anal region at the base.
b. Contents: The fossae primarily contain adipose, which allows for distension during passage of fecal matter and provides further support to the anal canal. The internal pudendal artery and vein, along with the pudenda! nerve, enter the ischioanal fossa by way of the lesser sciatic foramen. In each fossa, this neurovascular bundle travels deep to the obturator internu fascia, although the pudenda! canal, and gives off branches to the inferior anal and perinea! structures.



|
|
|
|
التوتر والسرطان.. علماء يحذرون من "صلة خطيرة"
|
|
|
|
|
|
|
مرآة السيارة: مدى دقة عكسها للصورة الصحيحة
|
|
|
|
|
|
|
نحو شراكة وطنية متكاملة.. الأمين العام للعتبة الحسينية يبحث مع وكيل وزارة الخارجية آفاق التعاون المؤسسي
|
|
|