النبات

مواضيع عامة في علم النبات

الجذور - السيقان - الأوراق

النباتات الوعائية واللاوعائية

البذور (مغطاة البذور - عاريات البذور)

الطحالب

النباتات الطبية


الحيوان

مواضيع عامة في علم الحيوان

علم التشريح

التنوع الإحيائي

البايلوجيا الخلوية


الأحياء المجهرية

البكتيريا

الفطريات

الطفيليات

الفايروسات


علم الأمراض

الاورام

الامراض الوراثية

الامراض المناعية

الامراض المدارية

اضطرابات الدورة الدموية

مواضيع عامة في علم الامراض

الحشرات


التقانة الإحيائية

مواضيع عامة في التقانة الإحيائية


التقنية الحيوية المكروبية

التقنية الحيوية والميكروبات

الفعاليات الحيوية

وراثة الاحياء المجهرية

تصنيف الاحياء المجهرية

الاحياء المجهرية في الطبيعة

أيض الاجهاد

التقنية الحيوية والبيئة

التقنية الحيوية والطب

التقنية الحيوية والزراعة

التقنية الحيوية والصناعة

التقنية الحيوية والطاقة

البحار والطحالب الصغيرة

عزل البروتين

هندسة الجينات


التقنية الحياتية النانوية

مفاهيم التقنية الحيوية النانوية

التراكيب النانوية والمجاهر المستخدمة في رؤيتها

تصنيع وتخليق المواد النانوية

تطبيقات التقنية النانوية والحيوية النانوية

الرقائق والمتحسسات الحيوية

المصفوفات المجهرية وحاسوب الدنا

اللقاحات

البيئة والتلوث


علم الأجنة

اعضاء التكاثر وتشكل الاعراس

الاخصاب

التشطر

العصيبة وتشكل الجسيدات

تشكل اللواحق الجنينية

تكون المعيدة وظهور الطبقات الجنينية

مقدمة لعلم الاجنة


الأحياء الجزيئي

مواضيع عامة في الاحياء الجزيئي


علم وظائف الأعضاء


الغدد

مواضيع عامة في الغدد

الغدد الصم و هرموناتها

الجسم تحت السريري

الغدة النخامية

الغدة الكظرية

الغدة التناسلية

الغدة الدرقية والجار الدرقية

الغدة البنكرياسية

الغدة الصنوبرية

مواضيع عامة في علم وظائف الاعضاء

الخلية الحيوانية

الجهاز العصبي

أعضاء الحس

الجهاز العضلي

السوائل الجسمية

الجهاز الدوري والليمف

الجهاز التنفسي

الجهاز الهضمي

الجهاز البولي


المضادات الميكروبية

مواضيع عامة في المضادات الميكروبية

مضادات البكتيريا

مضادات الفطريات

مضادات الطفيليات

مضادات الفايروسات

علم الخلية

الوراثة

الأحياء العامة

المناعة

التحليلات المرضية

الكيمياء الحيوية

مواضيع متنوعة أخرى

الانزيمات
The Wonderful World of Microbiology
المؤلف:
Gallagher ,J.C. and MacDougall ,c.
المصدر:
Antibiotics Simplified
الجزء والصفحة:
24-3-2016
5535
The Wonderful World of Microbiology
Despite the promises of the household-products industry, almost every surface is covered in microorganisms almost all the time. Swab a countertop, your skin, or your dinner and you will find a little world and that covers only the estimated 10% of bacteria that can be cultured! Obviously, trying to sterilize our patients (and our countertops) is futile; we have to try to target the bad organisms and let the rest happily crawl all over us.
In the microbial world, bacteria lie toward the “less like us” end of the spectrum (Figure 1 ). They are prokaryotes, not eukaryotes like fungi, protozoa, and humans. Viruses are even more different from us—they are basically just a package of genetic instructions in a protein coat (Figure 2 ). Differences between cells of microorganisms and humans in anatomy, biochemistry, and affinity of antibiotics for their targets are what allow for the safe and efficacious use of antibiotics. In this sec-tion we will concentrate on the microbiology of bacteria. Discussion of the unique characteristics of fungi, viruses, mycobacteria, and parasites will be covered in the sections where agents active against those organisms are introduced.

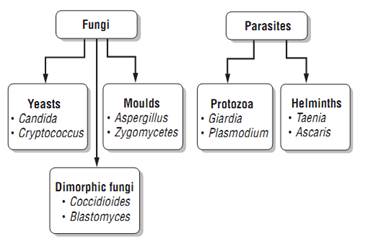
Figure 1 :The Microbial World
Differentiating bacteria that are responsible for infection from those just along for the ride can be difficult. Many bacteria that can cause human disease are also normal commensal flora, including Escherichia coli, Streptococcus pneumoniae, and Staphylococcus aureus. Thus, growth of one of these organisms from a culture is not necessarily synonymous with infection. Suspicion of infection is in-creased greatly if the organism grows from a normally sterile site, such as the bloodstream or cerebrospinal fluid (CSF). Indicators of infection in non-sterile sites (such as sputum and wound cultures) are a high number of organisms, presence of inflammatory cells, and symptoms referable to the culture site (e.g., cough or dyspnea in a patient with a sputum culture growing S. pneumoniae, redness and pain in a patient with a skin culture growing S. aureus).
Definitive identification and susceptibility testing may take anywhere from hours to months, de-pending on the organism and the methods used. Microscopic examination and staining may allow for rapid preliminary identification. For bacteria, the most important of these techniques is the Gram’s stain. Being able to interpret preliminary results of microbiology testing will allow you to pro-vide the most appropriate therapy to your patients as early as possible.

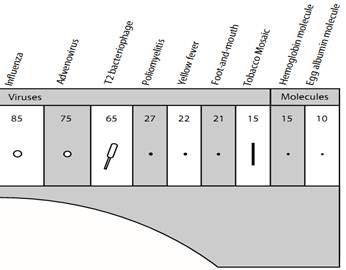
Figure 2 : Relative Sizes of Microorganisms
One of the most fundamental differences among types of bacteria is how they react to a Gram’s stain. Gram’s stain (crystal violet) is a sub-stance that selectively stains the cell walls of Gram-positive bacteria but is easily washed away from Gram-negative bacteria. Why? In Gram-positive bacteria, the outermost layer is a thick layer of peptidoglycan, a cellular substance that gives bacterial cells rigidity. In contrast, Gram- negative bacteria have an outer membrane of lipopolysaccharides that blocks the stain from adhering to the peptidoglycan within the cell (Figure3 ). Gram-negatives also contain peptidoglycan, but in smaller amounts, and it is not the outermost layer of the cell. Both Gram-positive and Gram-negative organisms contain an inner cell membrane that separates the cell wall from the cytoplasm of the organism.

Figure 3: Cell Walls of Gram-Positive and Gram-Negative Organisms
Figure 4 and Figure 5 show how you can identify different bacteria by differences in morphology, oxygen tolerance, and biochemical identification.

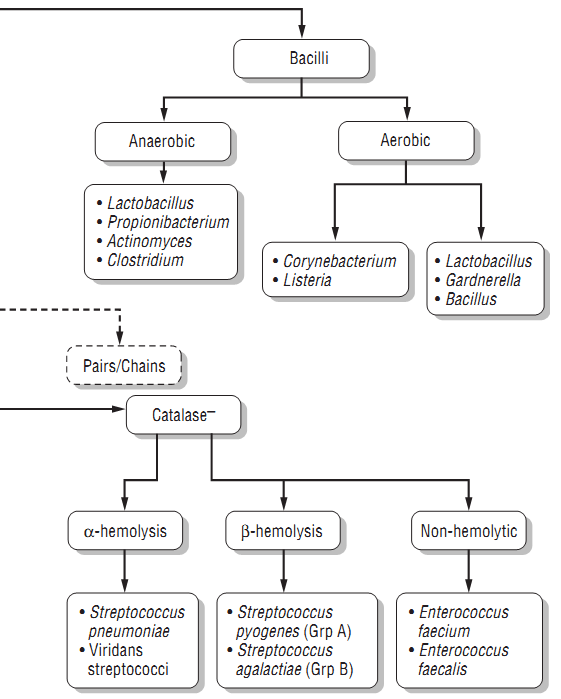
Figure 4 : Gram-Positive Bacteria
Rapid identification of Gram-positive bacteria based on morphology and preliminary biochemical tests can help to direct therapy.
1. Morphology: Most medically important Gram-positive pathogens are cocci (spheres) rather than bacilli (rods). The finding of Gram- positive bacilli should be interpreted within the clinical context: in blood cultures, Gram-positive bacilli often represent common skin contaminants (such as Propionibacterium, Corynebacterium, and Bacillus species). Detection of Gram-positive bacilli from necrotizing wound infections suggests clostridial infection, whereas the finding of Gram-positive bacilli in CSF cultures raises the concern for Listeria.
2. Colony clustering: Within the Gram-positive cocci, the staphylococci tend to form clusters, whereas the streptococci (including enterococci) typically appear in pairs or chains. Again, the clinical context aids in interpretation: The finding of streptococci in a respiratory culture suggests S. pneumoniae, while a report of “streptococci” from an intra-abdominal culture suggests Enterococcus (which may be identified preliminarily as a Streptococcus).
3. Biochemistry and appearance on agar: The rapid catalase test helps to differentiate staphylococci from streptococci. The coagulase test is useful for differentiating the more virulent (coagulase-positive) S. aureus from its cousin the coagulase-negative S. epidermidis. S. epidermidis is a frequent contaminant of blood cultures; if only one of a pair of blood samples is positive for coagulase-negative staphylococci, treatment may not be required. The pattern of hemolysis (clearing around colonies on agar plates) helps to differentiate among the streptococci: the oral flora ( α-hemolytic S. pneumoniae and the viridans strep); pathogens of the skin, pharynx, and genitourinary tract (β-hemolytic Group A and B strep); and the bugs of gastrointestinal origin (non-hemolytic enterococci: the more common E. faecalis and the more resistant E. faecium).
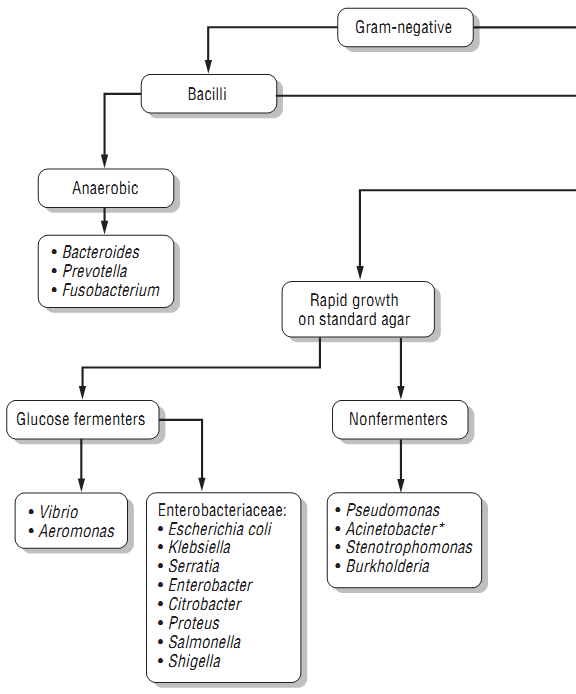
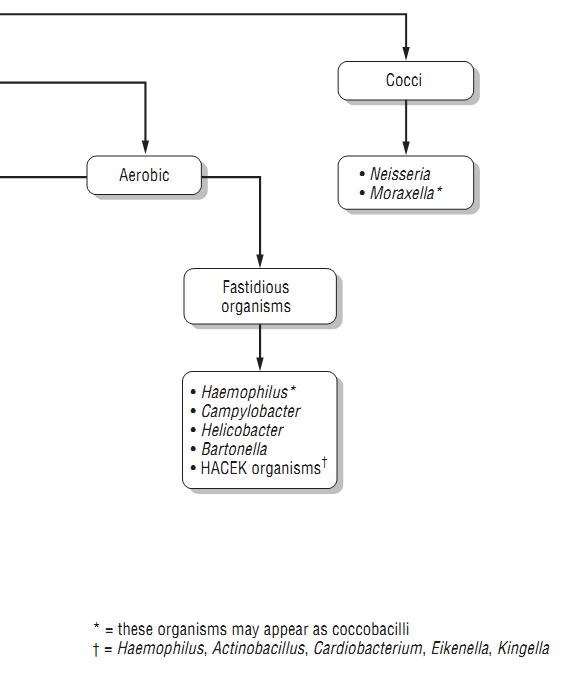
Figure 5: Gram-Negative Bacteria
Preliminary identification is somewhat less useful with the Gram-negative bacteria because more extensive biochemical tests are usually needed to differentiate among them.
1. Morphology: Among Gram-negative pathogens, the bacilli predominate. The situation in which identification of Gram-negative cocci would be most useful is in the setting of meningitis, where this finding would strongly suggest Neisseria meningitidis. Note also that some organisms have an intermediate or “coccobacillary” appearance, which may suggest H. influenzae, Moraxella, or Acinetobacter.
2. Glucose/lactose fermentation: The pathogens within the family Enterobacteriaceae (including E. coli, Klebsiella, Serratia, Proteus, and Enterobacter) generally ferment glucose/lactose; at this point the lab may identify them as “enteric Gram-negative rods.” In contrast, Pseudomonas, Acinetobacter, Stenotrophomonas, and Burkholderia are “non-fermenters”; a report of “non-fermenting Gram-negative rods” should lead you to reassess and if necessary broaden your antibiotic coverage, because these organisms have in common a high level of antibiotic resistance.
3. Fastidious organisms: These organisms are picky eaters—they grow slowly and often require specially supplemented media. Thus, it may take a few days to a few weeks for them to grow from culture
References
Gallagher ,J.C. and MacDougall ,c. (2012). Antibiotics Simplified. Second Edition. Jones & Bartlett Learning, LLC.
 الاكثر قراءة في مواضيع عامة في المضادات الميكروبية
الاكثر قراءة في مواضيع عامة في المضادات الميكروبية
 اخر الاخبار
اخر الاخبار
اخبار العتبة العباسية المقدسة

الآخبار الصحية











 قسم الشؤون الفكرية يصدر كتاباً يوثق تاريخ السدانة في العتبة العباسية المقدسة
قسم الشؤون الفكرية يصدر كتاباً يوثق تاريخ السدانة في العتبة العباسية المقدسة "المهمة".. إصدار قصصي يوثّق القصص الفائزة في مسابقة فتوى الدفاع المقدسة للقصة القصيرة
"المهمة".. إصدار قصصي يوثّق القصص الفائزة في مسابقة فتوى الدفاع المقدسة للقصة القصيرة (نوافذ).. إصدار أدبي يوثق القصص الفائزة في مسابقة الإمام العسكري (عليه السلام)
(نوافذ).. إصدار أدبي يوثق القصص الفائزة في مسابقة الإمام العسكري (عليه السلام)