

النبات

مواضيع عامة في علم النبات

الجذور - السيقان - الأوراق

النباتات الوعائية واللاوعائية

البذور (مغطاة البذور - عاريات البذور)

الطحالب

النباتات الطبية


الحيوان

مواضيع عامة في علم الحيوان

علم التشريح

التنوع الإحيائي

البايلوجيا الخلوية


الأحياء المجهرية

البكتيريا

الفطريات

الطفيليات

الفايروسات


علم الأمراض

الاورام

الامراض الوراثية

الامراض المناعية

الامراض المدارية

اضطرابات الدورة الدموية

مواضيع عامة في علم الامراض

الحشرات


التقانة الإحيائية

مواضيع عامة في التقانة الإحيائية


التقنية الحيوية المكروبية

التقنية الحيوية والميكروبات

الفعاليات الحيوية

وراثة الاحياء المجهرية

تصنيف الاحياء المجهرية

الاحياء المجهرية في الطبيعة

أيض الاجهاد

التقنية الحيوية والبيئة

التقنية الحيوية والطب

التقنية الحيوية والزراعة

التقنية الحيوية والصناعة

التقنية الحيوية والطاقة

البحار والطحالب الصغيرة

عزل البروتين

هندسة الجينات


التقنية الحياتية النانوية

مفاهيم التقنية الحيوية النانوية

التراكيب النانوية والمجاهر المستخدمة في رؤيتها

تصنيع وتخليق المواد النانوية

تطبيقات التقنية النانوية والحيوية النانوية

الرقائق والمتحسسات الحيوية

المصفوفات المجهرية وحاسوب الدنا

اللقاحات

البيئة والتلوث


علم الأجنة

اعضاء التكاثر وتشكل الاعراس

الاخصاب

التشطر

العصيبة وتشكل الجسيدات

تشكل اللواحق الجنينية

تكون المعيدة وظهور الطبقات الجنينية

مقدمة لعلم الاجنة


الأحياء الجزيئي

مواضيع عامة في الاحياء الجزيئي


علم وظائف الأعضاء


الغدد

مواضيع عامة في الغدد

الغدد الصم و هرموناتها

الجسم تحت السريري

الغدة النخامية

الغدة الكظرية

الغدة التناسلية

الغدة الدرقية والجار الدرقية

الغدة البنكرياسية

الغدة الصنوبرية

مواضيع عامة في علم وظائف الاعضاء

الخلية الحيوانية

الجهاز العصبي

أعضاء الحس

الجهاز العضلي

السوائل الجسمية

الجهاز الدوري والليمف

الجهاز التنفسي

الجهاز الهضمي

الجهاز البولي


المضادات الميكروبية

مواضيع عامة في المضادات الميكروبية

مضادات البكتيريا

مضادات الفطريات

مضادات الطفيليات

مضادات الفايروسات

علم الخلية

الوراثة

الأحياء العامة

المناعة

التحليلات المرضية

الكيمياء الحيوية

مواضيع متنوعة أخرى

الانزيمات
Limiting Clotting : Inactivating proteins
المؤلف:
Denise R. Ferrier
المصدر:
Lippincott Illustrated Reviews: Biochemistry
الجزء والصفحة:
6-1-2022
1767
Limiting Clotting : Inactivating proteins
The ability to limit clotting to areas of damage (anticoagulation) and to remove clots once repair processes are underway (fibrinolysis) are exceedingly important aspects of hemostasis. These actions are performed by proteins that inactivate clotting factors either by binding to them and removing them from the blood or by degrading them and also by proteins that degrade the fibrin meshwork.
Inactivating proteins
Proteins synthesized by the liver and by the blood vessels themselves balance the need to form clots at sites of vessel injury with the need to limit their formation beyond the injured area.
1. Antithrombin: Antithrombin III (ATIII), also referred to simply as antithrombin (AT), is a hepatic protein that circulates in the blood. It inactivates free FIIa by binding to it and carrying it to the liver (Fig.1). Thus, ATIII removes FIIa from the blood, preventing it from participating in coagulation. [Note: ATIII is a serine protease inhibitor, or “serpin.” A serpin contains a reactive loop to which a specific protease binds. Once bound, the protease cleaves a peptide bond in the serpin causing a conformational change that traps the enzyme in a covalent complex. α1-Antitrypsin is also a serpin.] The affinity of ATIII for FIIA is greatly increased when ATIII is bound to heparin, an intracellular glycosaminogly-can released in response to injury by mast cells associated with blood vessels. Heparin, an anticoagulant, is used therapeutically to limit clot formation. [Note: In contrast to the anticoagulant warfarin, which has a slow onset and a long half-life and is administered orally, heparin has a rapid onset and a short half-life and requires intravenous administration. The two drugs are commonly used in an overlapping manner in the treatment (and prevention) of thrombosis.] ATIII also inactivates FXa and the other serine proteases of clotting, FIXa, FXIa, FXIIa, and the FVIIa–TF complex. [Note: ATIII binds to a specific pentasaccharide within the oligosaccharide form of heparin. Inhibition of FIIa requires the oligosaccharide form, whereas inhibition of FXa requires only the pentasaccharide form. Fondaparinux, a synthetic version of the pentasaccharide, is used clinically to inhibit FXa.]
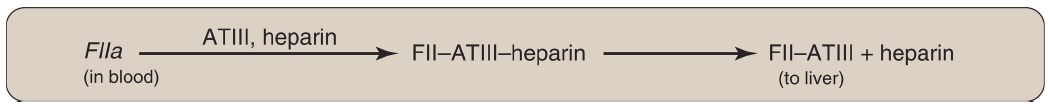
Figure 1: Inactivation of FIIa (thrombin) by binding of antithrombin III (ATIII) and transport to the liver. [Note: Heparin increases the affinity of ATIII for FIIa.] a = active; F = factor.
2. Protein C–protein S complex: Protein C, a circulating Gla-containing protein made in the liver, is activated by FIIa complexed with thrombomodulin. Thrombomodulin, an integral membrane glycoprotein of endothelial cells, binds FIIa, thereby decreasing FIIa’s affinity for fibrinogen and increasing its affinity for protein C. Protein C in complex with protein S, also a Gla-containing protein, forms the activated protein C (APC) complex that cleaves the accessory proteins FVa and FVIIIa, which are required for maximal activity of FXa (Fig. 2). Protein S helps anchor APC to the clot. Thrombomodulin, then, modulates the activity of thrombin, converting it from a protein of coagulation to a protein of anticoagulation, thereby limiting the extent of clotting. Factor V Leiden is a mutant form of FV (glutamine is substituted for arginine at position 506) that is resistant to APC. It is the most common inherited cause of thrombophilia in the United States, with highest frequency in the Caucasian population. Heterozygotes have a 7-fold increase in the risk for venous thrombosis, and homozygotes have up to a 50-fold increase. [Note: Women with FV Leiden are at even greater risk of thrombosis during pregnancy or when taking estrogen.]
Figure 2: Formation and action of the APC complex. Gla = γ- carboxyglutamate; a = active; F = factor.
Thrombophilia (hypercoagulability) can result from deficiencies of proteins C, S, and ATIII; from the presence of FV Leiden and antiphospholipid antibodies; and from excess production of FII (G20210A mutation). [Note: A thrombus that forms in the deep veins of the leg (deep venous thrombosis, or DVT) can cause a pulmonary embolism (PE) if the clot (or a piece of it) breaks off, travels to the lungs, and blocks circulation.]
 الاكثر قراءة في الكيمياء الحيوية
الاكثر قراءة في الكيمياء الحيوية
 اخر الاخبار
اخر الاخبار
اخبار العتبة العباسية المقدسة

الآخبار الصحية















 قسم الشؤون الفكرية يصدر كتاباً يوثق تاريخ السدانة في العتبة العباسية المقدسة
قسم الشؤون الفكرية يصدر كتاباً يوثق تاريخ السدانة في العتبة العباسية المقدسة "المهمة".. إصدار قصصي يوثّق القصص الفائزة في مسابقة فتوى الدفاع المقدسة للقصة القصيرة
"المهمة".. إصدار قصصي يوثّق القصص الفائزة في مسابقة فتوى الدفاع المقدسة للقصة القصيرة (نوافذ).. إصدار أدبي يوثق القصص الفائزة في مسابقة الإمام العسكري (عليه السلام)
(نوافذ).. إصدار أدبي يوثق القصص الفائزة في مسابقة الإمام العسكري (عليه السلام)


















